Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
Discogenic Pain - Diagnosis and Treatment
This is the first of three articles on lumbar discogenic pain. I suspect most of us are familiar with a classic disc herniation that causes sciatica. I will focus on axial discogenic pain, in which the back pain is primary. These articles will outline a comprehensive approach to treating this area, including assessment and diagnosis; treatment directly aimed at the disc space and the surrounding joints; and muscular function.
Most of our chronic low back pain (LBP) patients have some degree of clinically significant damage to one or more lumbar discs, ranging from moderate-to-severe degenerative changes to bulged, herniated or internally disrupted discs.
Most clinicians are familiar with what a bulged or herniated disc refers to, but may not be familiar with another disc problem, which can be called a torn disc, subligamentous herniation or internally disrupted disc. In a torn disc, the nucleus is not properly contained by the annulus, due to tears going into the annulus. These tears may be radial, circumferential or both. The tears are still contained by the outer layers of the annulus, so there are no nuclear fragments outside the container of the disc. These tears allow the nuclear material to push outward, creating pressure on parts of the annulus that are pain-sensitive, creating back pain. The irritation of the nerves in the annulus can create referred pain down to the groin, into the buttock and down the thigh. The classic signs of disc herniation will be absent. There are usually no changes in deep tendon reflexes, sensation, or muscle strength indicators, with normal toe flexor and extensor strength.
This pressure or leakage from the nucleus against the annulus may set up chemical changes, causing constant irritation and thus, constant pain. In other cases, the symptoms may only occur with increased biomechanical pressure, creating pain only while sitting or standing, or with flexion (or flexion combined with lifting or twisting). Prolonged sitting, or a sudden episode caused by an unguarded flexion or lifting movement, can create prolonged inflammation, initiating a painful episode that may last days to weeks, or more. The sudden episode is probably caused by a sudden nuclear leakage: a searing pain brought on because the nucleus has herniated farther into the annulus. This may be what happens to some of our patients who say, "I bent over, and my back went out."

Discogenic Pain Assessment
What might make us suspect an internally disrupted disc is contributing to the patient's problem? Here are seven signs or signals:
- Low back pain, worse after prolonged sitting or standing.
- Pain that refers to the buttock or groin, or down the leg; usually limited to above the knee.
- Chronic muscle imbalance patterns.
- We can observe similar phenomena in the spinal joints. They will sublux or fixate, secondary to the discal irritation. It may be in a predictable pattern on a particular individual, or may be somewhat more random. They will not hold their adjustments.
- History of the patient's lower back problems usually will show repeated episodes of low back pain. The onset may be sudden, after trauma or flexion with rotation motions, or may result from overuse or unidentified causes. The keys include the repetitive nature of the episodes. Another key is that they will usually fear or be unable to flex during the episodes.
- A straight leg raise will be limited on the side of buttock or groin pain. Especially in a chronic discal irritation, the dura and nerve root will be irritated on the involved side, and the hamstring will shorten. There will both be an absolute difference in SLR, and a feeling of restriction and tightness that occurs at an earlier point in the leg lift on that side.
- Unfortunately, all of the findings above can occur with any chronic lower back pain, whether it's from the facets, the SI, or the disc. Interspinous tenderness seems to be a key physical exam finding that points to the disc space as the pain generator. Over the inflamed disc level, the interspinous space, or the inferior aspect of the superior spinous process, will be quite tender. An interesting series of articles have been published describing a method of assessing the disc via spinous process tenderness, using a modified Oral-B electric toothbrush to create vibration in the interspinous space. This bony vibration stimulation was found to correlate well with discograms. Laverne Saboe's article on the Chiroview Web site reviewed this methodology. I have this tool, but have found it somewhat cumbersome.
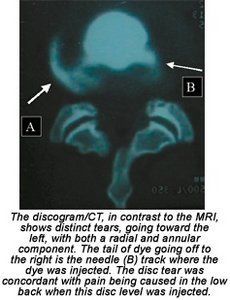
The discogram/CT, in contrast to the MRI, shows distinct tears, going toward the left, with both a radial and annular component. The tail of dye going off to the right is the needle (B) track where the dye was injected. The disc tear was concordant with pain being caused in the low back when this disc level was injected.After conversing with several other practitioners, and using this test on hundreds of patients, I have settled on a manual test. I call it the "digital interspinous pressure"(DIP) test. I believe I am testing for discitis, an irritated disc, with digital pressure. I assess the L5-S1, L3-L4 and L4-L5 spaces routinely. The pressure is applied with the edge of my thumb pad at the level of the interspinous space, pressing anterior and superior up toward the superior spinous process. I press deeply into the interspinous space, then attempt to lift the superior spinous cephalad. Some patients are exquisitely sensitive to even mild pressure; others require substantial pressure to elicit tenderness. If the annulus is completely torn, the disc container has lost its internal pressurization, so the test is likely to be negative. When the test is positive for tenderness, there is also a sense of restriction; a sense of vertical compression between the two contiguous vertebrae.
The DIP test is not perfect; it just gives us a sense of irritation at the level of the disc. The only way to research this would be to compare the results of this test to a discogram, which I have rarely ordered. Here is what I know with certainty as a clinician: The DIP sign correlates well with chronic lower back pain, and resolving the midline tenderness makes a difference in patients' recovery. What can cause this tenderness sign? One cause can be an internally disrupted or torn disc - but other biomechanical problems can create "false positives" on this test. This makes me suspect that the disc may be a pain generator for this patient, but the midline tenderness is really secondary to another biomechanical stress. In a "false positive" I will find one or two tender levels with digital interspinous pressure. I then fix what I find, e.g., I correct the lumbar restrictions, the sacroiliac, and the feet or hips. When I come back to the interspinous space, it is no longer tender. I interpret this to mean that the interspinous tenderness was a form of referred pain. The disc was under stress, due to other mechanical torques or restrictions, putting excessive tension into the disc space.
In a true positive on the DIP, I'll make my other corrections, come back to the interspinous space, and find that it is still exquisitely tender. This tells me I need to address the disc/interspinous space directly via vertical decompression. Those of you who have a vertebral distraction pump, or a flexion distraction table, already know how to do this. Our next article will review my protocol for treating the inflamed disc level. For those who can't wait, a rough draft of the next article is posted on my Web site.
The DIP test is useful for determining the prognosis by testing for interspinous tenderness on repeat visits. If the tenderness disappears after correction, and doesn't reoccur, it probably means the problem has a good prognosis. The problem is likely to be more biomechanical, and the patient usually recovers rapidly. If the tenderness continues to recur every time I examine this area, it makes me suspect substantial anatomical damage, probably to the disc, and/or a severely inflamed area. In these cases, the pain will take longer to resolve, and the prognosis is more guarded.
I hope I have given you some new questions, some new ways to think about chronic lower back pain. The spine is a three-joint complex, and our assessment and treatment must address the midline, as well as the facets.
Resources
- Vanharanta H, Ohnmeiss D, Aprill C. Clin J Pain 14:239-247, 1998.
- Yrjama M, Tervonen 0, Kurunlahti M, Vanharanta H. Bony vibration stimulation test combined with magnetic resonance imaging. Can discography be replaced? Spine 1997;22(7):808-13.
- Vanharanta H, Ohnmeiss D, Aprill C. Vibration pain provocation can improve the specificity of MRI in the diagnosis of symptomatic lumbar disc rupture. Clin J Pain 14:239-247, 1998.
- Saboe LA Jr. Chiroview Broadcast #1, Non-Invasive Provocative Vibratory Stimulation Test: Application for Discogenic Pain Without Radiculopathy. [url=http://www.chiroviewpresents.com/email_sub.htm]http://www.chiroviewpresents.com/email_sub.htm[/url].
- Personal conversation with Michael Karasec, MD, on digital pressure testing of the inflamed disc.
- www.spinaldiagnostics.com/sdx/frameset.html. (This is an excellent, lengthy article by Richard Derby on discography and other spinal injection procedures, on a site that is quite informative.)



