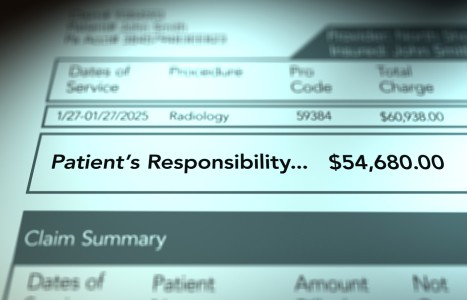
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
JMPT - Abstracts for May 2003 • Volume 26 - Number 4
Is low-back pain part of a general health pattern, or is it a separate and distinctive entity? A critical literature review of comorbidity with low-back pain.
Lise Hestbæk, DC; Charlotte Leboeuf-Yde, DC, MPH, PhD; Claus Manniche, DrMedSc
Introduction: Traditionally, research concerning the development of low-back pain (LBP) has focused on risk factors in search of explanations. This review focuses on comorbidity as a first step in identifying a frail subpopulation with a higher risk of developing LBP, in particular, persistent LBP. Research into comorbidity might yield a greater understanding of the underlying mechanism for this condition.
Data sources: Medline was searched from the beginning of the database to December 2000, followed by a search through the authors' personal collections of epidemiologic literature regarding LBP. All articles written in English were included if they related LBP to at least one other physical disorder. Articles were excluded if the prevalence of such disorders could not be compared to that of a control group or to the expected prevalence in a normal population.
Data extraction: The retrieved articles were evaluated for quality, based on predefined methodological criteria, whereupon information about associations between LBP and other physical disorders was extracted.
Results: Twenty-three articles were included. They showed positive associations to all disorders investigated (headache/migraine, respiratory disorders, cardiovascular disease, general health and others) with the exception of diabetes. There was little information regarding temporality, therefore, there are no clues as to causal mechanisms.
Conclusion: The literature leaves no doubt that diseases cluster in some individuals, and that low-back pain is part of this pattern. However, the nature of the relationship between LBP and other disorders is still unclear.
Key indexing terms: Low-back pain; comorbidity; headache; respiratory disorders; cardiovascular disease; general health.
Somatovisceral response following osteopathic HVLAT: A pilot study on the effect of unilateral lumbosacral high-velocity, low-amplitude thrust technique on the cutaneous blood flow in the lower limb.
Agust Karason, DC, Ian Drysdale, DO
Introduction: Spinal manipulative treatment is widely used among manual therapists, although knowledge regarding the absolute physiological effects has not been clearly established. In this study, 20 healthy males underwent a unilateral high-velocity, low-amplitude thrust (HVLAT) to the lumbosacral junction, while their cutaneous blood flow in the corresponding dermatome of the lower limb was monitored.
Methods: Subjects underwent a sham manipulation before the actual manipulation and acted as their own control group. Laser Doppler flowmetry was used to measure relative changes in the cutaneous blood flow over the L5 dermatome for five minutes before the sham manipulation; five minutes between the sham and the actual manipulation; and five minutes after the spinal adjustment. ANOVA and Tukey post hoc analysis was used in the interpretation of the data.
Results: Twelve nonsmoking subjects, all of whom received a successful HVLAT manipulation, showed a significant increase (p<0.001) in blood perfusion, both ipsilaterally and contralaterally. Six smokers responded with a significant decrease in blood flow ipsilaterally (p<0.01) and contralaterally (p<0.001) after HVLAT manipulation.
Conclusion: The results from this study support previous published hypotheses that spinal adjustments outside the region of the sympathetic outflow result in an increase in cutaneous blood flow. Further studies will be needed to confirm the outcome of this study, and more knowledge is needed regarding the specific neurophysiological effects of spinal manipulation.
Key indexing terms: Autonomic nervous system; osteopathy; somatovisceral reflex.
Interobserver reliability of the 24-hour schedule in patients with low-back pain: A questionnaire measuring the daily use and loading of the spine.
Eric Bakker; Hans Koning, Arianne Verhagen, PhDc; Bart W. Koes, PhD
Background: Low-back pain (LBP) is a major health problem in Western industrialized countries. The 24-hour schedule is an instrument designed to obtain insight in the use (i.e., posture and applied load) of the back. It consists of a questionnaire, a series of photos and a registration form.
Objective: To assess the interexaminer reliability of the 24HS in patients with LBP.
Study design: Reliability study.
Methods: People with LBP were included in the study. Sample-size calculation indicated that 40 participants would be sufficient in order to answer the research question. Participants were coded to remain anonymous, and after giving informed consent, they completed a questionnaire. Two trained examiners assessed each participant independently; a total of five examiners participated in the study.
Results: Forty participants were analysed. In our study population, the use of the back was approximately 10 times more in a flexed position compared to a lordotic position. Flexed activity was registered in all 80 assessments, but in 39 assessments, there was no registration of any activity in a lordotic posture. In only one participant (diagnosed with Bechterew's disease) was the use of the back more in a lordotic than a flexed posture. The intraclass correlation coefficient of the assessment was 0.81 (95% confidence interval = 0.67-0.89), corresponding with a high level of agreement between the examiners.
Conclusion: The interobserver reliability of the 24HS appeared to be high.
Key indexing terms: Interexaminer reliability; low-back pain; examination.
Comparison of dynamic posteroanterior spinal stiffness to plain-film radiographic images of lumbar disc height.
Christopher Colloca, DC; Tony Keller, PhD; Terry Peterson, DC; Daryn Seltzer, DC
Background: Assessments of spinal stiffness have become more popular in recent years as a noninvasive objective biomechanical means to evaluate the human spine. Studies investigating posteroanterior (PA) forces in spinal stiffness assessment have shown relationships to spinal level, body type, and lumbar extensor muscle activity. Such measures may be important determinants to discriminate between low-back-pain patients and asymptomatic subjects.
Objective: To determine the relationships between dynamic PA spinal stiffness and radiographic measures of lower lumbar disc height and disc degeneration.
Methods: L4 and L5 posterior disc height (PDH), posterior vertebral body height (PVH), anterior disc height (ADH), and anterior vertebral body height (AVH) were obtained from digitized plane film AP and lateral radiographs of 18 symptomatic LBP patients presenting to a chiropractic office (eight females and 10 males; 15-69 years of age; mean age 44.3; SD 15.4 years). Disc degeneration (DD) and facet arthrosis (FA) were assessed qualitatively from the films by an independent examiner. Anterior disc height ratios (ADHR=ADH/AVH) and posterior disc height ratios (PDHR=PDH/PVH) were calculated from the disc height measurements, and were compared to L4 and L5 posteroanterior spinal stiffness obtained, using a previously validated mechanical impedance stiffness assessment procedure.
Results: One-third of the subjects were found to have radiographic evidence of mild or moderate DD, and approximately two-thirds of the subjects showed signs of mild or moderate FA. The L4 and L5 anterior disc height and posterior disc height were approximately one half and one fifth, respectively, of each AVH, and the PA stiffness was greater at L4 than at L5. Male subjects had a greater ADHR than female subjects, but female subjects had a greater L4 and L5 PA stiffness in comparison to males; however, these differences were not statistically significant. Posteroanterior L5 vertebral stiffness was found to be significantly correlated to the L5 PDHR.
Conclusions: Computations of spinal input impedance are relatively simple to perform; can provide a noninvasive measure of the dynamic mechanical behavior of the spine; appear to have potential to discriminate pathologic changes to the spine; and warrant further study on a larger sample of normal subjects and patients.
Key indexing terms: Biomechanics; chiropractic; degeneration; intervertebral disc; mechanical impedance; radiography; spine; stiffness.
Herbal and nutrient supplementation practices of chiropractic patients: an Australian case study.
Jennifer Jamison, MB, BCh, PhD, EdD
Background: Escalating interest in alternative health care has resulted in increased use of nutritional supplements and herbs by consumers. A number of these neutraceuticals interact with prescription drugs, and may have adverse effects.
Objective: This study explores the extent to which chiropractic patients are likely to inform their chiropractic practitioners of their "medication" practices.
Method: A case study that included patients attending 21 chiropractic clinics (in five states and the Australian Capital Territories) was administered. Seven hundred fifty-eight patients provided information on their nutritional and herbal supplementation practices. Data was collected using a questionnaire that inquired about general lifestyle and sought particular information about self-initiated and professionally recommended medication practices. A list of "medications" that could influence coagulation was provided. Patients were specifically requested to indicate whether they had informed their chiropractor about any of these medications, herbs or nutrients they were taking.
Results: More than one in three chiropractic patients in this study were taking, either on the advice of a health professional or, more often, on their own initiative, nutritional supplements or herbs. However, chiropractors were only occasionally informed about the "medication" practices of their patients.
Conclusion: In view of the potential health risks and drug interactions, chiropractors should routinely inquire whether their patients are taking herbs or nutritional supplements.
Key indexing terms: Chiropractic; dietary supplements; herbs; coagulation.
The course of low-back pain in a general population. Results from a five-year prospective study.
Lise Hestbæk, DC; Charlotte Leboeuf-Yde, DC, PhD; Marianne Engberg, PhD; Torsten Lauritzen, DrMed Sc; Niels Bruun; Claus Manniche, DrMedSc
Objectives: To investigate the course of low-back pain (LBP) in a general population over five years.
Design: Prospective, population-based survey by postal questionnaires in 1991, 1992 and 1996.
Setting: The municipality of Ebeltoft, Denmark.
Subjects: 2,000 people, 30-50 years of age, representative of the Danish population.
Main outcome measure: Number of days with low-back pain (LBP) during the past year.
Results: Of the 1,370 recruited, 813 (59%) were followed for five years. The responders could be divided into three groups with regard to LBP: no pain, short-term pain and long-lasting/recurring pain. More than a third of people who experienced LBP in the previous year did so for >30 days. Forty percent of people with LBP >30 days at baseline remained in that group one and five years later, and 9% with LBP >30 days in year zero were pain-free in year five. People with LBP in year zero were four times more likely to have LBP in year one, and twice as likely to be affected in year five.
Conclusions: Low-back pain should not be considered transient, and therefore neglected, since the condition rarely seems to be self-limiting, but merely presents with periodic attacks and temporary remissions. On the other hand, "chronicity" as defined solely by the duration of symptoms should not be considered chronic.
Key indexing terms: Low-back pain; prognosis; natural history; prospective study.
Chiropractic care of a patient with vertebral subluxation and Bell's palsy.
Joel Alcantara, DC; Gregory Plaugher, DC; Darwin Van Wyngarden, DC
Objective: To describe the chiropractic care of a patient medically diagnosed with Bell's palsy and discuss issues clinically relevant to this disorder, such as its epidemiology; etiology; diagnosis; care; and prognosis.
Clinical features: A 49-year-old Caucasian female with a medical diagnosis of Bell's palsy sought chiropractic care for her complaints associated with this disorder. The patient's symptoms included a right facial paralysis, extreme phonophobia, pain in the right temporomandibular joint (TMJ) and neck pain. Signs of cervical vertebral and TMJ subluxations included edema, tenderness, asymmetry of motion and posture, and malalignment from detected plain-film radiographs.
Intervention and outcome: The patient was cared for with full-spine, contact-specific, high-velocity, low-amplitude adjustments (Gonstead technique) to sites of vertebral and occipital subluxations. The patient's left TMJ was also adjusted. The initial symptomatic response to care was positive, and the patient made continued improvements during the six months of care.
Conclusion: There are indications that patients suffering from Bell's palsy may benefit from a holistic chiropractic approach that not only includes a focus of examination and care of the primary regional areas of complaint (e.g., face, TMJ), but also potentially from significant vertebral subluxation concomitants.
Key indexing terms: Bell's palsy; temporomandibular joint; chiropractic.