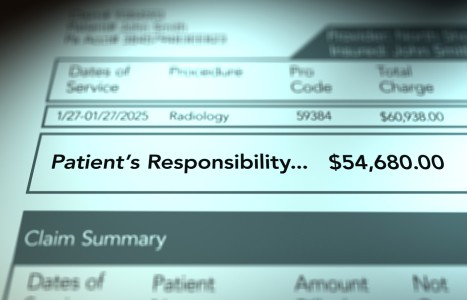
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Avoid Random Treatment of Trigger Points (Part 2)
Editor's note: Part 1 of this article appeared in the March 1 issue.
We must acknowledge that the fascia, which surrounds literally everything in our bodies, including every muscle fiber, is more than just a covering. The deep fascia is a communicating system due to the presence of increased amounts of proprioceptors and mechanoreceptors found in it. Receptors in superficial fascia and in the retinacula surrounding joints are also very much part of this communicating system.
Fascia is now considered a sensory organ communicating with the central nervous system.9 Due to the presence of proprioceptive and mechanoreceptive organs within the fascia, every time the fascia is stretched during muscle contraction or by passive muscle / fascial stretch, the force of the muscle contraction and the status of the muscle regarding its tone, movement, rate of change in muscle length and position of the associated body part is transmitted to the CNS by way of spindle cells.
The big news, as I have noted previously, is that these spindle cells are within the intramuscular fascia. The fascia is clearly a sensory organ regulating the function of muscles, and is the chief connector of connective tissue. Therefore, it is extremely important that spindle cells be allowed to stretch and shorten during muscle contraction in order to provide feedback to the CNS. For this to occur, the intermuscular fascia which houses these cells must be free to glide; otherwise, spindle cell function will be inhibited.
Stecco created a biomechanical model10 of the fascial system which includes myofascial units (MFU) that control specific joint movements. Each functional section of the body (14 segments) – cervical, thoracic, hip, leg, etc. – is controlled by MFUs. Each MFU is responsible for controlling a specific movement, and contains motor units that innervate mono- and biarticular muscle fibers responsible for moving a joint in a particular direction.
Within each of the MFUs are centers of coordination (CCs), which are the active component of the MFU. Myofascial tension or forces converge at the CCs, where part of the epimysial fascia is free to slide over the underlying muscle fibers and over muscle bellies; and where a majority of the spindle cells are located, usually distal from a joint. There are other points called centers of fusion which synchronize MFUs; they are located over tendons and retinacula, providing feedback by Golgi tendon organs.
Many of these CCs are also related to particular acupuncture points located in the fascia. Abnormal CCs represent densified fascia that can be palpated. To effectively treat these points, enough time has to be spent to completely restore gliding11 – usually around three minutes.
It is necessary to palpate the connection areas. Previous surgery, trauma and overuse almost always disrupt the fascia, affecting its proprioceptive function; and eventually may cause an adverse proximal or distal effect. It is essential that a complete case history be taken to determine past involvements, many of them completely forgotten.
Often after that 10-year-old ankle sprain (their lower back pain started nine years ago, for no apparent reason), the patient is completely unaware of their dormant ankle problem until you run some functional tests and compare the injured ankle with the normal side. Palpation of the fascia in the old injured ankle and leg will invariably show tender, densified areas the patient was never aware of. Treatment of a particular fascial pathway from the ankle to the knee, pelvis and lumbar spine can restore normal proprioception and end a perpetual incoordination.
In this biomechanical model, 10 myofascial pathways have to be evaluated for each joint. This is not as complicated as it may sound, since a complete knowledge of these points allows for a quick evaluation.
The anatomy of the myofascial system points to the presence of myofascial kinetic chains. An important paper on myofascial continuity in the anterior region of the upper limb was authored by A. Stecco,12 in which he describes an anatomical myofascial relationship and location of areas to treat by fascial manipulation:
"Stecco C also studied this chain13 and described the "'anatomical continuity' between the various muscles involved in the movement of flexion of the upper limb. This study demonstrated the existence of specific myofascial expansions, with a nearly constant pattern, which originate from the flexor muscles and extend to the overlying fascia. The clavicular part of the pectoralis major sends a myofascial expansion, with a mean length of 3.6cm, to the anterior region of the brachial fascia, and the costal part sends one to the medial region of the brachial fascia (mean length: 6.8cm). The biceps brachii presents two expansions: the lacertus fibrosus, oriented medially, with a mean height of 4.7cm and a base of 1.9cm, and a second, less evident, longitudinal expansion (mean length: 4.5cm, mean width: 0.7cm). Lastly, the palmaris longus sends an expansion to the fascia overlying the thenar muscles (mean length: 1.6cm, mean width: 0.5cm). During flexion, as these muscles contract, the anterior portion of the brachial and antebrachial fascia is subject to tension. As the fascia is rich in proprioceptive nerve endings, it is hypothesized that this tension activates a specific pattern of receptors, contributing to perception of motor direction. If the muscular fascia is in a non-physiological state, these mechanisms are altered, and the proprioceptors in the fascia may be incorrectly activated, thus giving rise to many types of extra-articular pain."
There are four MFUs in the anterior arm with a CC in each unit. There are also MFUs for backward motion, internal and external rotation and medial and lateral directions. Both functional testing and palpation of CCs for density determine which line of MFUs (sequences) may be involved.
It is very possible that the painful shoulder did not have any densified CC, while the forearm and elbow area had densified, painful CCs. Treatment of the hand and elbow without treatment of the painful shoulder could resolve the shoulder pain.
This patient may have had a history of a wrist fracture or a chronic elbow tendinosis. This scenario could be possible throughout the body. The patient may have been previously treated for a tender area in the shoulder, but the palpation of densified tissue within the chain is more important than patient tenderness – although they usually coincide. The densification refers to a lack of proper fascial gliding which adversely affects the proprioceptors and mechanoreceptors, causing improper muscle function and eventual pain.
It becomes apparent that if we are treating someone using a mechanical load, the load to be exerted on abnormal tissue should be determined by palpation, rather than the area of pain. More and more, I notice patients pointing to their painful area where the tissue is loose and gliding.
Palpation becomes our chief method of evaluation before we decide where to exert pressure. This concept also applies to spinal palpation, of course: We release what is fixed, rather than the area of the patient's complaint.
References
9. Hammer WI. "The Fascial System Is a Sensory Organ." ACA News, 2014:15-20.
10. Stecco L, Stecco C. Fascial Manipulation, Practical Part. Piccin Nuova Libraria, Padova, Italy, 2009.
11. Borgini E, Stecco A, Day JA, Stecco C. How much time is required to modify a fascial fibrosis? J Bodyw Mov Ther, 2010 Oct;14(4):318-25.
12. Stecco A, Macchib V, Stecco C, Porzionato A, Day JA, et al. Anatomical study of myofascial continuity in the anterior region of the upper limb. J Bodyw Mov Ther, 2009 Jan;13(1):53-62.
13. Stecco C, Gagey O, Macchi V, Porzionato A, et al. Tendinous muscular insertions onto the deep fascia of the upper limb. First part: anatomical study. Morphologie, 2007 Mar;91(292):29-37.