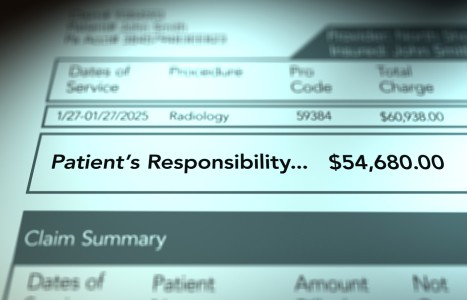
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Interdigital Neuritis
Also known as Morton's neuroma, interdigital neuritis results from entrapment of one or more of the interdigital nerves, which are branches of the medial and lateral plantar nerves. The most common early symptoms of this condition include a tingling between the toes and a feeling of fullness between the involved metatarsal heads. Affected individuals frequently complain that their socks are "bunched" in the forefoot and that the discomfort is reduced when the shoes are removed.
Over time, a thick neuroma may form that increases the likelihood of chronicity because the thickened nerve is more readily pinched. Apparently, no part of the nerve is protected from the trauma, and histological findings include epi-, peri- and endoneural fibrosis. Clinically, it is often possible to identify a neuroma by squeezing the forefoot at the metatarsal heads and feeling for the presence of a Mulder's click: a clunk-like sound that can be palpated, which occurs when a swollen intermetatarsophalangeal bursa is displaced.
While this condition may occur at any of the interdigital nerves, the nerve located between the third and fourth metatarsal is the most frequently injured. Although it was originally claimed that the nerve in this interspace was more often involved because it receives fibers from both the medial and lateral plantar nerves (which was believed to make it thicker), this theory has been disproved, since all of the interdigital nerves are approximately the same diameter.1

Until recently, the most popular theory regarding the origin of interdigital neuritis/neuroma was that dorsiflexion of the toes during the propulsive period tethered the interdigital nerves against the deep transverse ligament. This theory was disproved by Kim, et al.,1 who performed meticulous dissections on 17 fresh, frozen cadavers to evaluate the relationship between interdigital neuromas and the deep transverse metatarsal ligament during the push-off phase of gait.
Because the authors demonstrate that the interdigital neuroma always forms distal to the deep transverse ligament, the nerve had to be compressed beneath the distal aspect to the involved metatarsal head and its proximal phalanx. (Fig. 1) This being the case, the most appropriate treatment is to lessen pressure at that site by incorporating metatarsal pads, bar posts, and/or a U-shaped balance placed beneath the specific metatarsal heads. (Fig. 2) This latter addition is especially important because it protects the distal metatarsal heads throughout the propulsive period.

An often-overlooked cause for the development of an interdigital neuritis is tightness in the gastrocnemius muscle. As demonstrated by DiGiovani, et al.,2 tightness in the gastrocnemius, not the soleus muscle, predicted a wide range of forefoot injuries, including metatarsalgia and metatarsal stress fractures. It is likely that tightness in the gastrocnemius muscle results in a premature lifting of the heel during the gait cycle, which may amplify forces centered beneath the metatarsal heads during the propulsive period.
Regardless of the mechanism, comprehensive treatment of an interdigital neuritis should always include various manual therapies to lengthen a tight gastrocnemius muscle. Several studies have shown that deep-tissue massage applied before stretching results in more rapid length gains.3-4
Because of their ability to distribute pressure away from the metatarsal heads, patients suffering with interdigital neuritis should also be evaluated for weakness of the digital flexors. Because a strong flexor hallucis longus distributes pressure away from the central metatarsal heads toward the great toe,5 adequate strength in this muscle is important in the treatment and prevention of interdigital neuritis. The easiest way to exercise flexor hallucis longus is to place an elastic band beneath the hallux while alternately dorsi and plantarflexing the great toe. Three sets of 40 repetitions are usually sufficient to strengthen the muscle.
Possibly because it alters the transfer of force through the foot,6 manipulation of the various joints of the foot and ankle should always be considered. According to Brantingham, et al.,7 manipulation of the metatarsophalangeal and calcaneocuboid joints is especially important. Another manual procedure that is often helpful when treating interdigital neuritis is to have the patient perform nerve glides after massaging the muscles that traverse the proximal pathway of the involved nerve. (Fig. 3) This technique may enhance the overall flexibility of the plantar nerves and their branches.
Finally, to reduce pressure centered beneath the metatarsal heads during daily activities, patients should be informed to avoid high heels and wear shoes with adequate room in the toe boxes. Runners presenting with this condition should switch to a rearfoot strike pattern, reduce their overall length of stride and maintain maximum ranges of ankle dorsiflexion.
By evaluating and correcting the various biomechanical factors affecting the involved nerves, even the most troublesome interdigital nerve injuries may respond favorably to conservative care.
References
- Kim J, Choi J, Park J, et al. An anatomical study of Morton's interdigital neuroma: the relationship between the occurring site and the transverse metatarsal ligament (DTML). Foot Ankle Int, 2007;28:1007-1010.
- DiGiovani C, Kuo R, Tejwani N, et al. Isolated gastrocnemius tightness. J Bone Joint Surg, 2002;(84A):962-971.
- Hopper D, Deacon S, Das S, et al. Dynamic soft tissue mobilization increases hamstring flexibility in healthy male subjects. Br J Sports Med, 2005;39:594-598.
- Guler-Uysl F, Kozanoglu E. Comparison of the early response to two methods of rehabilitation for adhesive capsulitis. Swiss Med Wkly, 2004;134:363-368.
- Ferris L, Sharkey N, Smith T, et al. Influence of extrinsic plantar flexors on forefoot loading during heel rise. Foot Ankle, 1995;16:464-473.
- Lopez-Rodriguez S, Fernandez de-las-Penas C, Albuquerque-Sendin F, et al. Immediate effects of manipulation of the talocrural joint on stabilomitry and baropodometry in patients with ankle sprain. J Manip Phys Ther, 2007;30:186-192.
- Brantingham J, Snyder W, Michaud T. Morton's neuroma. J Manip Phys Ther, 1991;5:317-322.