Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
What to Do About Refund Requests
There is a rapidly growing and disturbing trend you may have noticed making its way toward your office. From the e-mails I receive, I have good reason to believe it is happening more frequently and indiscriminately - regardless of where you practice, how you practice or whom your primary payers are. For most chiropractors, in addition to being just plain irritating, the appropriate reaction to this phenomenon is a bit perplexing.
While this description may fit a number of our practice pests, the bugger that is our specific focus today is refund requests. Like a small flesh wound, many DCs wonder how to handle this irritant. Do you just ignore it, leave it alone and hope it will go away? Do you seek professional attention? Do you fight back or pay it back? Before I propose some specific strategies on how to handle these refund requests, let's discuss the nature and identification of these beasties.
Incorrect Payments
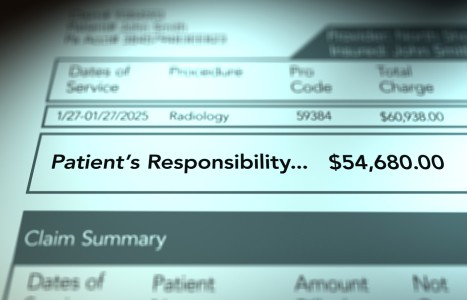
The most common variety of refund requests involves payers attempting to get their money back for what they have determined to be an "incorrect payment." Over the past several years, third-party payers have begun to increase their recruitment of external auditing companies to review their claims processing.
As these audit companies are paid contingency fees on the amount of money they can help the insurance companies recover, it's no surprise these audit companies are willing to look high and low for any potential payment errors and submit a demand for repayment as a result. Thus, the sudden proliferation of refund requests that malign your mailbox.
Don't Sign the Check ... Yet
Before you write that refund check to the insurance company, there are a few details you might wish to review. Most states require that the payer state the reason for the overpayment request. In other words, it's not simply enough for a payer to say, "Oops, we overpaid you. Please refund our money." Legally, they may be required to give the specific rationale for which the overpayment was determined. In many cases, this can be done looking at claim data (what was present on the claim you submitted) to determine if there were errors in regards to incompatible billing codes, exhausted benefits and other problems that clue the audit company in to the fact that they believe you have been overpaid.
Regardless of their rationale, you want to request the details of why you are receiving the request so that you can verify whether it is accurate or if there are points to dispute.
Due and Owing
Another critical element to examine is your insurance carrier's payment policies. Some carriers' contracts have reimbursement policy language that includes the terms due and owing. Minus the legalese, this means that if the carrier's policy says the chiropractor has to do X, Y and Z to get paid, and that is what you did, then the benefits are "due and owing." In other words, you fulfilled your end of the bargain, so you deserve to be paid - whether or not some outsourced audit company argues about the finer details of what you should have been paid after the fact. As you may imagine, knowledge of this type of contractual arrangement can become very handy in rapidly rejecting many refund requests.
Other Reasons to Reject a Refund Request
Another common reason to reject refund requests is if the request is a dispute over the extent or existence of coverage for the treatment. For example, the payer may try to request a refund on the basis that it processed the claim in error. Perhaps the benefits had already been exhausted, a referral or precertification was required but not obtained, or the amount should have been applied to the patient's deductible.
In short, if the insurance company cites its own mistake in applying benefits, hang on to your checkbook. There are several court cases that have recognized the provider's right to dispute a refund request when the insurance company is at fault regarding the processing of its own payments. Essentially, the courts have ruled that health care providers who are innocent and act in good faith without prior knowledge of the mistake are due their just wages.
Where to Go for More Help
To wrap things up, we've discussed three distinct situations in which the request for a refund should be denied: a) the company wrongly requested a refund for properly billed, documented and rendered services; b) the insurance is contractually bound to honor your payment because you met its policy requirements; or c) the refund request was made as a result of a dispute of a coverage issue in which the insurance company incorrectly applied benefits.
Based on the scenarios discussed above, many providers should not refund requested benefits to the insurance carrier immediately, as it appears these situations are very common reasons that refunds are requested. Instead, each refund request should be researched to determine the accuracy of the payment in question. This may require seeking additional information from the carrier and patient regarding benefits. You may have to dig out your provider contract to see what their reimbursement policy language states. Or you might have to be a little savvy in the legal arena to determine whether the payer has exceeded the time frame in which it can even request a refund.
So, if you have been feeling persecuted as a chiropractor or have been wondering if payers are trying to "nickel and dime" you to death with the multitude of mini-refund requests (many are for small amounts under $250), you are definitely not alone. The situation is so commonplace among all health care providers that many states have enacted laws regarding refund attempts.
But don't just sit there letting this whole scenario boil your blood pressure. If you believe a refund request was made in error, send a written response to the carrier explaining why you won't be giving them their money back. For a sample of a "Refund Request Rejection Letter," send me an e-mail at info@strategicdc.com, noting that you read this article, and I will be glad to provide you with an example you can use.
Finally, if you are unable to resolve the dispute and still feel that the insurance company is unjustly requesting its money back, law firms that specialize in health care law typically can assist providers in determining their right to retain disputed benefit payments. Depending on the amount and frequency of the refund requests, sometimes legal action is the most effective way to retain your hard-earned income and put a stop to this threat to your practice's bottom line.