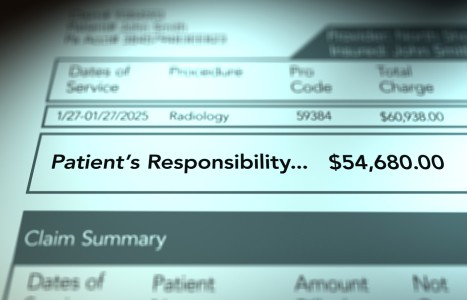
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Our Shrinking Chiropractic Practice Box
Yesterday I received an advertisement from Dr. Louis Sportelli that promoted the "American Academy of Manipulative Therapy" and its Spinal Manipulation Institute Newsletter. James Dunning, DPT (along with a string of other designations) is listed as "institute faculty." This is all about teaching people how to learn spinal manipulation, specifically the "high-velocity, low-amplitude thrust manipulation," as they call it. If you review the organization's Web site ([url=http://www.spinalmanipulation.org]http://www.spinalmanipulation.org[/url]), you will see that what they are teaching looks very much like what we teach and practice.
This is just one of many examples of how others who called spinal manipulation "quackery" just a few decades ago have now become the "originators" of this form of therapy. From every quarter, people outside the chiropractic profession are learning how to use spinal manipulation. How does the chiropractic profession respond? With the same answers and methods used by the allopathic profession when it tried to "contain and eliminate the chiropractic profession," namely, "Let's sue them and get legislation to stop them!"
The reality is a lesson we should have learned when we won the Wilk v AMA lawsuit back in 1987. We cannot stop people from learning, even if it hurts our pride and our pocketbooks. We fall back on the same ineffective "need to protect the patient" argument the AMA used against us, but in the final analysis, nothing we do of that nature will change the inexorable movement of others into what we see as "our turf."
Two Schools of Thought
As I observe the profession, I see those who believe no one but the chiropractor can truly know how to "correct subluxation," so there is nothing to worry about as long as we can convince people to sign up for lifelong "chiropractic corrective adjustments." These people believe correcting the subluxation improves vitality and promotes "wellness."
There are those who are well-educated on the application of "evidence-based practice" and who, therefore, have concluded that all the chiropractic physician can properly do is take care of people with a limited list of spinal and, in some instances, extremity concerns. Furthermore, they conclude, this is how society sees the chiropractic profession, so it makes no sense to try to go in any other direction. These are the self-proclaimed "experts in spinal care."
Both of the groups described above think their version of chiropractic practice is the right one and should be how chiropractic medicine is defined. I see things differently. Those in the first group usually don't complain about reimbursement because they typically charge cash - usually a lower fee - and depend on convincing a lot of people to buy into their version of "wellness." This is successful in many instances, but is unsupported by any legitimate evidence grounded in science, and depending upon the population density, can result in a gradual decline in practice as people become more and more aware of how the particular practice functions. One of the most frequently voiced complaints about chiropractic practice is, "Once you go to one (DC), they keep you coming back over and over."
The members of the second group make a legitimate case that if the chiropractic profession wishes to be "mainstreamed," it must be part of mainstream reimbursement processes. That might be a legitimate assumption, but in my daily interactions with many practicing chiropractic physicians, one of the most often heard complaint relates to continuing decline in reimbursement.
There are numerous reasons, apparently, but fundamentally, the third-party payers do not see what the chiropractic physician has to offer as being vital to the needs of the patient. The same services can be acquired from any number of other providers who do similar procedures. Furthermore, one wonders if becoming part of the "mainstream" at a time when that very system is clearly falling apart is the right way to go.
Another Way
I think there is another way, and I believe that more and more people are interested in and ready for it. This is not to suggest that it is easy, but then, what about health care practice is today? I think the future in chiropractic medicine is in the arena of what we used to call "general chiropractic practice." Granted, today it is referred to as "primary care," but even that definition varies depending upon who is using it.
The argument against "general chiropractic practice" I hear from the chiropractic profession is this: "Chiropractic physicians are not adequately educated to practice 'primary care.'" I hear that chiropractic physicians have not done thousands of prostate examinations, or looked into thousands of eyes or listened to thousands of hearts, and on and on. In some instances that is true, but it should not be an indictment of the entire profession.
What are the fundamentals of "primary care/general chiropractic practice?" The formation of the doctor/patient relationship is the beginning, followed by the ability to do a thorough patient history, perform vital signs and complete a comprehensive physical examination such that a working diagnosis can be reached. This is a starting point for any kind of treatment.
Following this, the chiropractic physician needs to decide the best treatment for the patient, which includes a decision regarding whether this patient needs the kind of care only an allopath or osteopath can provide, or whether, with appropriate use of all the tools available to the chiropractic physician, the patient could be reasonably expected to respond to chiropractic medicine.
This is exactly what we did when I graduated 40 years ago, and most often, we ended up treating the patient using the methods we had learned. Yes, often that involved the use of manipulative procedures, because these methods have far-reaching positive effects on people with many health issues. We also recommended therapeutic exercise, lifestyle changes, postural training, dietary modifications, nutritional supplementation and botanicals.
We used braces and casts for simple fractures. We used ice and sometimes heat, and we utilized various forms of physiotherapeutic procedures. We tested for food allergies and changed diets accordingly, often seeing dramatic improvements in our patients' complaints. And we recognized that the best any physician can hope to accomplish is to help the patient return to optimal health - not perfect health. We realized that, as Dr. Janse used to say, "Even the most elegant health care procedures and efforts all end in the same place - the end of life."
In two recent issues of Dynamic Chiropractic, Don Petersen, editor/publisher, suggested that perhaps it is time for us to consider (reconsider) primary care as a practice profile. It pleased me to see this because it suggests more and more people of influence are seeing the value of and need for this kind of approach.
I was recently contacted by a professor from a major university who was writing a paper for the Institute of Medicine summit regarding integrative medicine [held in late February 2009]. It is her position that chiropractic and naturopathic physicians, as well as doctors of Oriental medicine, should be included as primary care providers. This from a thinker outside our profession.
All current statistics point to a rapidly growing deficiency of primary care providers in this country for a number of reasons. At the same time, doctors of nursing practice and others are trying vigorously to move in to fill the need for primary care doctors. While the allopaths are protesting this kind of move, they offer no real solution, either. Meanwhile, we as a profession continue to argue among ourselves about our proper place in the grand scheme of things.
Time to Expand the Practice Box
For me the picture is clear: Health care delivery in the United States is not working as it currently exists. There are many problems, but one of the most significant ones is that many people do not have family doctors who develop doctor/patient relationships or provide basic diagnosis and treatment of fundamental health issues.
To make matters worse, those kind of doctors, who come from the allopathic and osteopathic ranks, are becoming few and far between. Chiropractic physicians, who, according to the Council on Chiropractic Education's Standards, have been educated as "primary care physicians," have a unique and clear opportunity to enter the void. Must we wait for some signal from the government? Must we gain approval from the allopathic profession? Neither scenario is likely, but we have the statutory and educational wherewithal to move ahead as providers of "general chiropractic medicine," and we should wait no longer to get started.
Do we need prescriptive rights? Perhaps, but for the most part we don't have them right now, and that should not deter us from taking the step into primary care. Are we covered by third parties? For the most part, probably not, but then we weren't in my practice days, either. Will patients pay a reasonable fee for care they are not able to get elsewhere? Many DCs say they won't, so it is our responsibility to educate them - and I think we can.
I recently saw an alumna who practices in an eastern state. I asked about practice - which she said is good. I asked about billing and her immediate response was, "It's mostly cash." I asked, "And patients are willing to pay?" Her reply was, "Yes, if you give them something they need and are not getting anywhere else, they will pay." She then went on to describe her "practice of general chiropractic medicine." I hear this more and more today, and am pleased to hear it.
It is time for us to quit reducing the size of our practice boxes. It is time to provide all that we did within the musculoskeletal box and much, much more. It is time for us to return to the practice of "general chiropractic medicine." It is time for us to return to the principle of "treating our patients as if they were our father, mother, brother, sister, spouse or child." If we return to these simple, basic principles, I believe we can not only survive, but also thrive as a profession, and many thousands more people who need the kind of care we can provide will benefit.