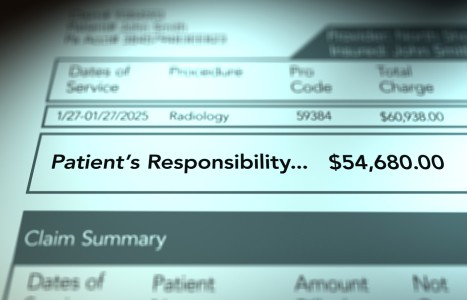
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Osteoporosis Essentials for Primary Health Care Providers
Approximately one in four women and one in eight men over the age of 50 develop osteoporosis. These are alarming statistics, as 25 percent of individuals who sustain an osteoporotic hip fracture die within the first year from related complications. In many cases, patients are admitted to the hospital after a hip fracture. Fluid can pool in their lungs, creating a ripe environment for bacteria to flourish. In such cases, they often develop pneumonia and die from the infection. This happens to be a very common scenario.
In Canada, more women die each year from the consequences of hip fractures than from breast and ovarian cancer combined.1 Studies indicate that much of this problem is preventable by using proper nutrition and lifestyle practices, including ingesting sufficient amounts of calcium, vitamin D, magnesium and protein, as well as other nutrients such as zinc, manganese, copper, silicon, soy isoflavones, vitamin K, folic acid as well as vitamin B6.
Studies suggest that, in particular, suboptimal intake of calcium and vitamin D account for a high percentage of osteoporosis cases. To prevent osteoporosis, the National Institutes of Health states that young men and women between the ages of 11 and 24 should consume 1,200 mg of calcium per day. For women ages 25 to 50, the recommendation is 1,000 mg per day; women over 50 (not using hormone replacement therapy) should increase their intake to 1,500 mg per day. Men between 25 and 65 years of age should consume 1,000 mg per day and increase their calcium intake to 1,500 mg per day after age 65. On average, the majority of adults in our society fall short of their daily calcium needs by at least 500 mg. As such, most people should increase their intake of calcium-rich foods (see calcium and vitamin D food charts below) and consider taking a high-potency multivitamin/mineral supplement that contains 500 mg of elemental calcium per day. In many cases, an additional bone-support supplement containing another 500 mg of calcium and other bone-support nutrients may be required to optimize osteoporosis prevention, based upon one's age and dietary patterns.
In the case of vitamin D, which is necessary for the absorption and utilization of calcium, a high-potency multivitamin/mineral supplement should contain 400 IU of vitamin D. This amount appears to be adequate up to age 40-45, at which point many osteoporosis and cancer experts suggest increasing vitamin D supplementation to 800-1,000 IU per day. This dosage has been shown to decrease hip fractures up to 43 percent and to increase vitamin D blood levels into a range associated with decreased risk of colon, breast and prostate cancer. Vitamin D stimulates the production of a carrier protein within intestinal cells that is responsible for the absorption of calcium from the intestinal tract into the bloodstream.
Once osteoporosis is present, diet, supplementation and exercise are not sufficient therapy. If osteoporosis has already developed, medical treatments beyond diet, exercise and supplementation may be necessary to prevent the occurrence or recurrence of bone fractures and related life-threatening consequences. This usually involves the use of antiresorptive drugs, which help to slow down the further loss of calcium from bone. For patients who have normal bone density or osteopenia (some bone loss, but not yet considered osteoporotic), nutrition, exercise and supplementation are the primary interventions that should be in place to prevent osteoporosis development. For this reason, it is imperative that you ensure a bone-density assessment has been performed on all patients who meet the inclusion criteria for bone-density evaluation. Only a bone-density assessment can determine if an individual has developed osteoporosis or if they are at high risk for developing this condition at some point in the near future.
As such, you should ask all of your patients the following questions. If they answer "yes" to any of the following questions, a bone-density assessment should be undertaken, if one has not been performed within the past two years.
- Are you a woman over the age of 50?
- Are you a woman who entered into early menopause (40-45) or premature menopause (before 40)?
- Are you a woman who has had both ovaries surgically removed before normal menopause (age 45-55)?
- Are you a woman under 45 years of age who routinely misses menstrual cycles or has greatly diminished menstrual flow due to estrogen and/or progesterone deficiency?
- Have you ever suffered from anorexia or bulimia?
| Table 1: Sources of Calcium From Common Healthy Foods | ||
| Food | Portion Size | Amount of Calcium (mg) |
| Low-fat yogurt | 1 cup | 415 |
| Low-fat milk (nonfat, 1%) | 1 cup | 300 |
| Low-fat cottage cheese | 1/2 cup | 75 |
| Sardines with bones | 3 oz | 370 |
| Salmon with bones (canned) | 3 oz | 165 |
| Processed tofu with calcium sulfate | 4 oz | 145 |
| Canned shrimp | 3 oz | 100 |
| Cooked lentils | 1 cup | 75 |
| Chicken breast | 3 oz | 10 |
| Tuna | 3 oz | 5 |
| Collard greens | 1/2 cup | 180 |
| Spinach | 1/2 cup | 85 |
| Stalk of broccoli | 1 medium | 70 |
| Orange | 1 medium | 55 |
| Green beans | 1/2 cup | 30 |
| Lettuce | 1/2 head | 15 |
| Orange juice | 1/2 cup | 10 |
| Apple | 1 medium | 10 |
| Whole wheat bread | 1 slice | 20 |
| Cooked spaghetti | 1 cup | 15 |
| Cooked rice | 1/2 cup | 10 |
| Apricots, raw, dried | 4-6 halves | 24 |
| Dates | 3-4 | 22 |
| Figs (canned) | 3 | 35 |
| Figs (dried) | 2 | 56 |
| Grapefruit | 1 medium | 40 |
| Prunes, dried, raw | 5 | 27 |
| Raisins | 1/4 cup | 31 |
| Raspberries | 2/3 cup | 40 |
| Strawberries | 1 cup | 42 |
| Roasted almonds | 1 oz | 80 |
| Kale | 1/2 cup | 47 |
| Baked beans | 1/2 cup | 78 |
| White beans | 1/2 cup | 96 |
| Dry-roasted soybean nuts | 1/2 cup | 232 |
| Table 2: Sources of Vitamin D From Common Healthy Foods | ||
| Food | Portion | Amount of Vitamin D (IU) |
| Low-fat cheese (less than 4% milk fat) | 3 1/2 oz | 12-15 |
| Halibut | 3 1/2 oz | 44 |
| Herring | 3 1/2 oz | 320 |
| Mackerel (raw) | 3 1/2 oz | 1100 |
| Salmon (fresh) | 3 1/2 oz | 450 |
| Salmon (canned) | 3 1/2 oz | 1300 |
| Shrimps | 3 1/2 oz | 150 |
| Oysters | 3-4 medium sized oysters | 5 |
| Nonfat, skim milk and 1% milk (vitamin D fortified) | 8 oz | 100 |
Are you a woman who, at some time in your life, exercised excessively or competitively to the point that your body fat was very low?
- Have you undergone treatment with oral glucocorticosteroid drugs (e.g., prednisone, cortisone) for more than three months at any time during your life?
- Have you ever been diagnosed with hyperparathyroidism?
- If you are a woman, did your mother or perhaps a sister develop osteoporosis?
- Are you a man over 65 years of age?
- Are you older than 45 and your doctor has told you that you are underweight?
- In general, do you have poor muscular development and strength?
- Have you ever taken anticonvulsant medication for more than two years?
Calcium and Vitamin D From Low-Fat Food Sources
The food charts included in this article provide values for calcium and vitamin D from healthy foods that are low in saturated fat. You may wish to have your patients fill out a seven-day diet history from which you can estimate their daily average of intake of these two vital bone-support and cancer-prevention nutrients. If daily intake falls short of the desirable levels for their age and gender, you should strongly consider setting out a strategy to help them acquire the missing levels of calcium and/or vitamin D from healthy food choices and/or supplementation as a crucial aspect of a disease prevention and longevity program. Ingesting sufficient and optimal amounts of calcium and vitamin D has the potential to extend a patient's life and greatly reduce the risk of certain life-threatening degenerative diseases such as osteoporosis and colon cancer (and in the case of vitamin D alone, breast and prostate cancer, as well as multiple sclerosis).
Note that other than vitamin D-fortified dairy products, the only other good source of dietary vitamin D is fish that feed on plankton living near the surface of the sea, which is exposed to sunlight. Sunlight, in turn, stimulates the production of vitamin D in plankton. Exposure of human skin to direct sunlight also stimulates the production of vitamin D within the skin. However, in cold climate areas (all regions north of the midpoint of the United States) there is insufficient sunlight intensity from October to May to produce vitamin D in the skin to any appreciable degree. Thus, individuals living in these areas of North America must pay special attention to acquiring optimal amounts of vitamin D from any combination of vitamin D-fortified dairy products, fish, seafood and vitamin D-containing supplements. The same is true for individuals living far south of the equator (in the Southern Hemisphere) in climates that have cold winters lasting more than two to three months.
Reference
- Osteoporosis Society of Canada. Clinical practice guidelines for the diagnosis and management of osteoporosis. Can Med Assoc J 1996;155:1113-33.
Other Resources
- Kinyamu HK. Dietary calcium and vitamin D intake in elderly woman: effect on serum parathyroid hormone and vitamin D metabolites. Am J Clin Nutr 1998;67:342-8.
- Dawson-Hughes B, et al. Rates of bone loss in postmenopausal women randomly assigned to one of two dosages of vitamin D. Am J Clin Nutr 1995;61:1140-5.
- Kreiger N, et al. Dietary factors and fracture in postmenopausal women: a case-control study. Int J Epidemiol 1992:21953-8.
- Chapuy, MC, et al. Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med 1992;327:1637-42.
- Dawson-Hughes B, et al. Effect of calcium and vitamin D supplementation on bone density in men and women 55 years of age and older. N Engl J Med 1997;337:670-677.
- Peters U, Chatterjee N, McGlynn A, et al. Calcium intake and colorectal adenoma in a U.S. colorectal early detection program. Am J Clin Nutr 2004;80:1358-65.
- Baron JA, Beach M, Mandel JS, et al. Calcium supplements for the prevention of colorectal adenomas. Calcium Polyp Prevention Study Group. N Engl J Med 1999;340:101-107.
- Optimal calcium intake: NIH consensus panel. JAMA 1994;272:1942-8.
- Nelson ME, et al. Effects of high intensity strength training on multiple risk factors for osteoporotic fractures: a randomized controlled trial. JAMA 1994;272:1909-14.
- Woo TCS, Choo R, Jamieson M, et al. Pilot study: potential role of vitamin D (cholecalciferol) in patients with PSA relapse after definitive therapy. Nutrition and Cancer 2005;5(1):32-36.