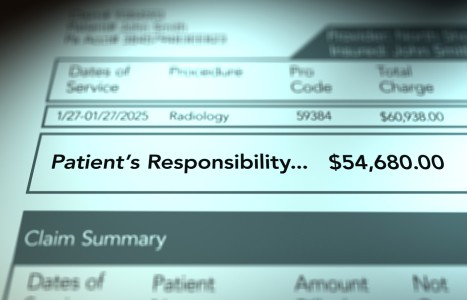
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
The Acute Chiropractic Index (ACI)
Medical necessity is one of those terms that you hear and immediately think you know what it means. However, when asked to define it, vague and blurry terms crop up. This is complicated by the fact that competing perspectives (insurers vs. physicians) may define the term narrowly or broadly.
This paper proposes the Acute Chiropractic Index (ACI) to quantify patient status by use of a point system. Third-party payers then have the option of defining medical necessity as any score over a certain threshold of points. This would allow a somewhat objective means of determining patient status without depending on diagnosis or orthopedic exam findings to document clinical necessity. An alternative to depending on diagnosis and exam findings to determine necessity of care is desirable because of the inconsistencies inherent in using these as guides for medical necessity. Every practitioner has been frustrated by using a diagnosis appropriately for minor conditions, which also appropriately fits a more severe case but does not communicate the difference in the two conditions.
The ACI is a way to quantify the variables as components of a standardized index. The ACI is composed of six separate assessments.
Acute Chiropractic Index
Pain Scale
The pain scale is the patient's subjective rating of discomfort on a scale of 1-10. This is in common clinical use and gives a measure of the patient's perception of their pain level. "1" is barely noticeable pain; "10" is the worst pain the patient has ever experienced.
The usefulness of this measurement is well-documented in the literature.
Oswestry Index
The Oswestry Disability Index for the lumbar spine is also in common clinical use, as is its cervical counterpart, the Modified Oswestry Disability Index. This measures the ability of patients to perform activities of daily 1iving or their impairment due to the spinal condition. It produces a score of 0 -100% where 0 represents no disability at all. A score of 100 would be totally disabled and incapacitated.
The Oswestry has been shown to be reproducible and especially useful when repeated indexes are compared over the course of time.
The usefulness of this measurement is also well-documented in the literature.
Positive Tests for Radiculopathy
These would include tests such as Laseque's straight leg raise, shoulder depressor, altered reflexes, and paraesthesias. The fact that there is inflammation of nerve tissue is a factor that deserves extra weighting because this tissue is so vital to functioning of the human organism. Additionally, this tissue is relatively slow to heal and often requires additional healing time and treatment.
Degenerative Changes
The presence of degenerative changes (spurs/spondylosis, degenerated discs, facet arthrosis, uncinate degeneration, etc.) deserves additional weighting because of the implication of scarred, fibrosed, and otherwise less than healthy soft tissues in and around the spine. These degenerated tissues are more easily injured and more difficult to rehabilitate.
Anomaly on X-Ray or Postsurgery
The altered biomechanics due to spinal anomalies is sufficient to allocate additional weighting to this finding. Examples of pertinent anomalies include (but are not limited to) nonsegmentation, spondylolisthesis, scoliosis, spina bifida occulta, and lumbarization/sacralization. For instance, spina bifida occulta at L5-S1 has been linked to increased risk of disc herniation.
Additionally, postspinal surgery patients have scar tissue in and around the spine and typically a reduction in the amount of normal tissue (such as in the removal of disc tissue).
Occupational/Lifestyle Stress Documented in History
Inclusion of this parameter is an attempt to allow for lifestyle and occupational activities that can exacerbate an injury or complicate/slow the healing process. Examples would be physical labor occupations such as brick masons, occupations that involve exposure to vibration such as truck and heavy machine operators, and occupations that require constant repetitive strain to the spine such as fork lift operators. This is by no means an all-inclusive list.
Implementation
There are two primary uses for this outcomes scale. The first is in educating the patient about their condition and the pertinent parameters that will be measured over the course of their care. This can be reported to the patient during the report of findings after each exam. In this way, communication with the patient is enhanced and reasonable expectations are set about how "success" will be defined and measured.
Secondly, third-party payers, who have always sought a way to measure clinical results, can use it. A potential use of this assessment would be to allow for a certain range of visits for scores within a certain range i.e.:
A new evaluation would be indicated after the initial program of care so that a new ACI score can be made. Requests for additional visits would have to be documented and supported by the most recent ACI.
Summary
By utilizing some commonly used measurements and emphasizing those clinical factors that most directly impact chiropractic outcomes, an index has been developed to assist doctors and third-party payers in measuring and assessing clinical success/failure as well as necessity of care. The ACI has the additional advantage of being a valuable patient education tool.
Acute Chiropractic Index
Note: The proposed index is only appropriate for use as an assessment of acute and symptomatic patients. It is not intended as a tool in monitoring maintenance, elective, or other non-symptomatic care. It is suggested that the physician utilize other common tools such as palpation, leg checks, etc., to determine necessity of nonsymptomatic care.
Joe Siragusa,DC,DABCO
Monroe, North Carolina