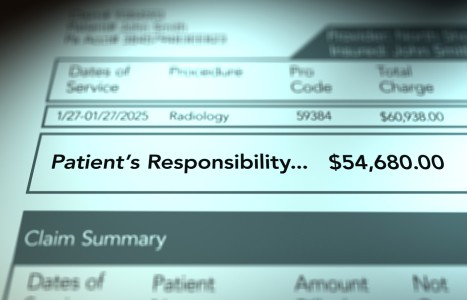
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
The Best of Times, the Worst of Times (Pt. 1)
- Despite the near-universal recognition of the benefits of chiropractic care, administrative burden and persistently low reimbursement have pushed many practices to the brink of economic viability.
- Two largely unseen forces that profoundly shape the environment in which DCs practice include medical loss ratio (MLR) and mental health parity.
- As a result, DCs face a practice environment that undermines their ability to thrive economically and compromises patient access to high-value non-invasive and non-pharmacological care recommended by clinical practice guidelines.
Editor's Note: This three-part article series is co-authored by Drs. Dave Elton, John Allenburg, Wayne Bennett, Marty Caron, Darren Chase, Molly Magnani, Ben McDowell, Melissa Naegre, Garret Rock, Robb Russell, and Mike Simone - all doctors of chiropractic. Access their LinkedIn pages for more information at the end of this article.
"It was the best of times, it was the worst of times, it was the age of wisdom, it was the age of foolishness...” This famous opening line from A Tale of Two Cities by Charles Dickens aptly captures the current state of the chiropractic profession.
A substantial body of high-quality research demonstrates the value of chiropractic care. Clinical practice guidelines consistently recommend the services provided by doctors of chiropractic (DCs) as a first-line option for spinal disorders and chronic musculoskeletal pain. Increasingly, medical physicians and other healthcare professionals seek to collaborate with DCs. As has been the case for over a century, patients report high satisfaction with their chiropractic experiences.
Despite the near-universal recognition of the benefits of chiropractic care, administrative burden and persistently low reimbursement have pushed many practices to the brink of economic viability, with patients experiencing the consequences of less access to high-value musculoskeletal care.
While worthwhile, additional practice guidelines and research are not sufficient catalysts for change. Without changes to how practices are organized, the technology supporting practices, and the systems that govern payment and network participation, such efforts are unlikely to meaningfully improve DCs’ ability to achieve the healthcare quadruple aim and sustainable care for more people.
We are at a pivotal time for the chiropractic profession, with both significant challenges and opportunities. The goal of this three-part series is to identify actions that will enable DCs to realize their full potential as an essential part of an effective, efficient and patient-centered healthcare system. We start the series by examining two largely unseen forces that profoundly shape the environment in which DCs practice.
Medical Loss Ratio (MLR)
The medical loss ratio (MLR) provision of the Affordable Care Act (ACA) requires health insurance companies to spend a minimum percentage of premium dollars on healthcare services and quality improvement activities, rather than on administrative costs, marketing and profits. The goal is to ensure consumers receive value for their premiums and to prevent excessive insurer profit or overhead spending.
For the large-group insurance market, insurance companies must allocate at least 85% of premium dollars to healthcare services or quality improvement activities. For the individual and small-group markets, the threshold is 80%. When insurers do not spend the full MLR on healthcare services or quality improvement activities, they are required to issue a rebate for the difference to policyholders.
At first glance, this seems like an appropriate consumer protection. However, a significant loophole exists. The MLR only applies to regulated insurance companies, not to healthcare services companies. It is estimated that between 25%-50% of commercial insurance premiums are shifted to unregulated healthcare services companies through a capitation loophole.
Capitation involves transferring a portion of premium dollars from an insurance company to a healthcare services business. While the entire capitation amount is counted as medical expense by the insurance company, helping meet the MLR threshold, once shifted to a healthcare services company, the same capitation payment is not subject to the MLR rebate provisions.
This means there are no limits to healthcare services business profits or overhead expenses. As a result, healthcare services businesses are free to set aggressively low fee schedules and impose administrative barriers to care such as prior authorization, retrospective audits and “tiering” programs.
Imagine a family paying $10.00 per lunch to a school lunch program. The school has a rule that at least $8.00 (80%) must go toward food and works with suppliers to provide high-quality options. Of the remaining $2.00, $1.75 goes to things like staff pay, plates and utensils, leaving a $0.25 profit. If a child chooses $7.00 worth of items, the family receives a $1.00 rebate from the school.
Now imagine the school uses an external food service company to manage the lunch program for the same $10.00. Due to a loophole, the food service company is not required to follow the $8.00 rule and works with suppliers to provide low-quality options for $5.00 per lunch. The same $1.75 is spent on staff pay, plates and utensils, leaving $3.25 profit for the food services company.
If due to the poor food quality, students select $2.00 worth of food, the food services company retains $6.25 as profit. For students choosing to purchase food directly outside the school, the food services company retains an $8.25 profit. The loophole introduces misaligned incentives whereby profit is emphasized over high-quality food.
The reason this is important for DCs is because one type of healthcare services business is the intermediary DC network, which began to appear in the late 1980s and early 1990s. Many, though not all, intermediary-insurer relationships involve capitation arrangements. The same insurance company may have both capitated and non-capitated arrangements with the same intermediary DC network. To simplify operations, intermediaries often apply the same fee schedules and utilization management strategies across all plans, regardless of whether a capitation arrangement exists.
Today, a small number of intermediaries manage DC networks for most commercial insurance companies, some federal programs, Medicare Advantage plans, some work comp insurers, and the Veterans Administration Community Care Network. This level of market consolidation combined with the MLR loophole has profound implications for DCs. (The cost and utilization control tactics, and their impact on the sustainability of DC practices, will be covered in part 2 of this series.)
Mental Health Parity
Mental health parity refers to laws requiring that mental health and substance use disorder (MH/SUD) benefits be treated equally to medical/surgical benefits.
The Mental Health Parity Act of 1996 (MHPA) first required parity in annual and lifetime dollar limits for MH/SUD versus medical/surgical benefits in large-group plans. The Mental Health Parity and Addiction Equity Act of 2008 expanded MHPA by mandating parity in financial requirements (such as copays and deductibles), and quantitative treatment limits (such as annual visit limit and prior authorization processes) between MH/SUD and medical/surgical services. The Affordable Care Act of 2010 (ACA) further extended these protections to individual and small-group markets, and designated MH/SUD services as essential health benefits.
MH parity laws are intended to prevent insurance companies and intermediaries from imposing stricter coverage limits, higher cost-sharing, or more burdensome authorization requirements on MH/SUD treatment than on comparable medical/surgical services. With insurance companies using tools like copays, deductibles, visit limits, and preauthorization to control the costs of MH/SUD treatment, MH parity laws require that these same cost-control tactics are applied to similar types of medical care.
Because chiropractic care, like mental healthcare, is relatively low-cost, outpatient and often involves frequent visits, it is commonly used as a medical service comparable to MH/SUD treatment. Even though chiropractic care makes up a small part of total healthcare spending, the same restrictions designed to manage the higher costs of MH/SUD care end up being applied to chiropractic care to comply with MH parity laws.
The Takeaway / What’s Next
DCs face a practice environment that undermines their ability to thrive economically and compromises patient access to high-value non-invasive and non-pharmacological care recommended by clinical practice guidelines.
Part 2 of this series will examine the specific tactics used by intermediary networks that restrict DCs from achieving their full potential to help patients. Part 3 will describe the vision, strategies and tactics the co-authors are collectively leading to enable practices to achieve the quadruple aim.
List of Co-Authors:
- Dave Elton (corresponding) dave@arete.healthcare LinkedIn Arete Healthcare
- John Allenburg LinkedIn ChiroCenter Chiropractic & Wellness
- Wayne Bennett LinkedIn Bennett Clinic
- Marty Caron Caron Chiropractic
- Darren Chase LinkedIn The Athlete Stop
- Molly Magnani LinkedIn IPGMN – Integrated Provider Group of Minnesota
- Ben McDowell LinkedIn McDowell Chiropractic
- Melissa Nagare LinkedIn Southern California University of Health Sciences
- Garret Rock LinkedIn Arete Healthcare
- Robb Russell LinkedIn Southern California University of Health Sciences
- Mike Simone LinkedIn Simone Physical Medicine