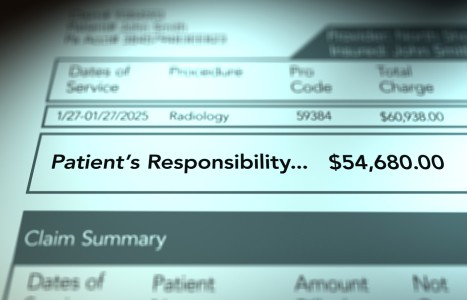
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
AK Manual Muscle Testing: As Reliable as the Deep Tendon Reflex?
Editor's note: This is the third in a series of three articles on applied kinesiology (three different authors);
Dr. Richard Belli's "Applied Kinesiology and the Motor Neuron" appeared in the April 21 issue; Dr. Scott Cuthbert's "Applied Kinesiology: How to Add Cranial Therapy to Your Daily Practice" appeared in the May 19 issue.
Manual muscle testing (MMT) was born in the 1950s with the work of two physical therapists (Kendall and Kendall) and their historic text, Muscles: Testing and Function.1 Since that time, this body of knowledge has been integrated into the standard procedures of orthopedists, neurologists and practitioners of physical medicine worldwide.6
In 1964, Goodheart2 began utilizing the methods of Kendall and Kendall in clinical practice to assess patterns of functional muscular inhibition ("weakness") and determine which treatment options, based on known neurophysiologic parameters, might be viable to restore proper muscular facilitation ('strength'). His clinical research marked the beginning of applied kinesiology (AK).
Since its inception, critics of AK MMT have questioned a host of its precepts. As a result, AK practitioners have undertaken efforts to address some of these issues; particularly, why the growing body of scientific data appears decidedly mixed. It is the assertion of applied kinesiologists that a number of past research designs, some of which gave little credence to the diagnostic merits of AK MMT, did not accurately reflect the principles and practice of AK as a functional neurological assessment.8
The interexaminer reliability of MMT has been one of these controversial topics. In a study by Lawson and Calderon,3 interexaminer reliability of AK MMT was found to be statistically significant for muscles that could be well-isolated, such as the pectoralis major, but less so for tests of muscle groups, such as the hamstrings. This study not only lends supporting evidence for the reliability and reproducibility of AK MMT, it reinforces a clinical observation of applied kinesiologists: When muscles can be well-isolated, the resultant outcomes appear to be more accurate than group muscle tests. Hence, applied kinesiologists are instructed to be cautious in their methods of isolating and testing muscles. Furthermore, gross MMT, as advocated by some, is not comparable with the sophisticated testing procedures of AK. This may be partially responsible for some of the conflicting evidence from past research designs.
In related problems of accuracy, the issue of fatigue also has been raised. Could the results of AK MMT be attributable to fatigue, especially when the examiner tests a given muscle repeatedly? In a study by Leisman, et al.,5 it was determined that muscles identified via AK MMT as inhibited are in a fundamentally different state than those identified as facilitated, and that the testing procedures can be evaluated objectively by quantifying the neurological electrical characteristics of muscles. Perhaps most importantly, it was established that these inhibition patterns were not attributable to fatigue.
Another common misconception about AK MMT is that the examiner simply employs more force when identifying an inhibited muscle, thus "overpowering" the subject. In a French study, the electrical activity in muscles was measured, as in the aforementioned Leisman study.5 Perot, et al.,9 found a significant difference in electrical activity of the muscle (corresponding to the outcome differences in muscles identified as facilitated or inhibited) with AK MMT. It further showed that these outcomes were not attributable to increased or decreased testing force applied by the doctor during the procedure.
Fundamentally, AK MMT is based on the theory that the testing procedures reflect changes in the central nervous system. When a subject is unable to respond adequately to an examiner's application of force in executing the manual muscle test, the muscle is identified as conditionally inhibited. At that point, a sensory, receptor-based stimulus, such as joint manipulation, can be introduced to determine whether said stimulus results in conditional facilitation of the muscle in question. If conditional facilitation is elicited, it is thought that the bias of the alpha motor neuronal pool, which supplies the muscle, shifts to a more normal, central integrative state. Consequently, AK MMT is thought to represent a clinical window of function of the central nervous system.10
Opponents argue that while this theory may adhere to well-established principles of neurophysiology and the basic sciences, the evidence is lacking. However, in another study by Leisman, et al.,4 changes in somatosensory-evoked potentials during AK MMT were elicited. This study measured the way the central nervous system functions when muscles are identified as facilitated or inhibited, and found clear, consistent and predictable differences in measurements of brain activity between outcomes. These findings support the contention that AK MMT reflects changes in the central nervous system.
Clinical experience dictates that although pathological lesions are often easily uncovered, functional neurological assessment remains complicated and problematic. An example of this is the reliability of deep tendon reflexes (DTRs). Despite their marginal reproducibility,7 they are well-accepted as standard procedures. The time-honored utilization of DTRs is still considered feasible for two reasons: a) the underlying mechanism is explicable; and b) their interpretation, when taken in context by a responsible practitioner, is invaluable. That is to say, a single aberrant DTR must be considered as one parameter in a greater clinical picture. In this respect, AK MMT is no different. The mechanisms appear to be explicable and no more esoteric than DTRs. Furthermore, responsible applied kinesiologists comprehend that not only is it obligatory to avoid overextrapolating the significance of a single manual muscle test, it is crucial that the procedures of AK be used in conjunction with other confirmatory diagnostic parameters, such as history, radiologic imaging and laboratory analyses. Failure to do so is an example of one of the many abuses of MMT.
Just as a DTR represents a "snapshot" of a spinal cord reflex loop, a manual muscle test is also a "snapshot." It is a clinical window of the central nervous system which, due to its plasticity, is constantly in flux. The only difference is that the manual muscle test is exceedingly more complex, not only in terms of its mechanism, but also in how well a doctor can be trained to perform it. That is where the science and the art must blend. The experienced neurologist will likely be more successful at eliciting an accurate DTR, and appropriately interpreting it in the context of an exam, than the family practice physician. By the same token, expert applied kinesiologists are better equipped with the psychomotor skills necessary to perform accurate MMT.7 In light of this, it is my opinion that the use of AK MMT, when understood as part of a greater clinical picture, can become standard procedure, as have DTRs.
References
- Kendall FP, Kendall-McCreary E, Provance P. Muscles: Testing and Function, 4th ed. Lippincott, Williams & Williams, 1993.
- Goodheart GJ. Applied Kinesiology Workshop Manual. Privately published. Detroit, Mich., 1964
- Lawson A, Calderon L. Interex-aminer agreement for applied kinesiology manual muscle testing. Percept Mot Skills, 1997 Apr;84(2):539-46.
- Leisman G, Shambaugh P, Ferentz AH. Somatosensory evoked potential changes during muscle testing. Int J Neurosci, 1989 Mar;45(1-2):143-51.
- Leisman G, Zenhausern R, Ferentz A, Tefera T, Zemcov A. Electromyographic effects of fatigue and task repetition on the validity of estimates of strong and weak muscles in applied kinesiological muscle-testing procedures. Percept Mot Skills, 1995 Jun;80(3 Pt 1):963-77.
- Magee DJ. Orthopedic Physical Assessment, 4th Ed. WB Saunders Co., 2002.
- Marshall GL, Little JW. Deep tendon reflexes: A study of quantitative methods. J Spinal Cord Med. 2002 Summer; 25(2):94-9.
- Motyka TM, Yanuck SF. Expanding the neurological examination using functional neurologic assessment, part I: methodological considerations. Int J Neurosci, 1999 Mar;97(1-2):61-76.
- Perot C, Meldener R, Goubel F. Objective measurement of proprioceptive technique consequences on muscular maximal voluntary contraction during manual muscle testing. Agressologie, 1991;32(10 Spec No):471-4.
- Schmitt WH, Yanuck SF. Expanding the neurological examination using functional neurologic assessment part II: Neurologic basis of applied kinesiology. Int J Neurosci, 1999 Mar;97(1-2):77-108.
Marcello Caso, DC, DIBAK
Sacramento, California