Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
Evaluating the TMJ: Imaging & Diagnostic Considerations
What is the most common cause of facial pain? Of course, one thinks of headaches and traumatic injuries; other causes include nerve conditions, jaw and dental problems, and infections. But the most common cause of facial pain is temporomandibular joint and muscle disorders.
TMJDs cause recurrent pain and dysfunction of the jaw joint and its associated muscles and supporting tissues. It is a musculoskeletal condition. TMJDs are the second most commonly occurring musculoskeletal disorder resulting in pain and disability. What's the first? Chronic lower back pain!
TMJDs affect approximately 5-12 percent of the population, with an annual cost estimated at $4 billion. About half to two-thirds of those with TMJ disorders will seek treatment. Among these, approximately 15 percent will develop chronic TMJD.1
There are data documenting chiropractic treatment of TMJDs.2-7 We need to make certain that these data are continually updated to document our results. We can only achieve this by appropriate imaging and documentation. Even case reports can prove to be invaluable in the gathering of data.
I am not an expert in the treatment of TMJDs. What I can contribute is this review of best imaging modalities available for the evaluation of this extremely complex joint.
Which Imaging Modality to Choose?
The diagnosis and management of temporomandibular disorders (TMD) require both clinical and imaging examinations of the temporomandibular joint. There are several modalities that can be used to image the TMJ, including magnetic resonance imaging (MRI), computed tomography (CT), cone beam CT, ultrasonography and conventional radiography. Imaging can be difficult, particularly when the patient is symptomatic, because it requires patient participation, i.e., opening and closing the jaw.
- Conventional radiography is of limited value. The use of flat plane films for TMJ pathology is not sufficient, because this joint requires 3-D imaging.
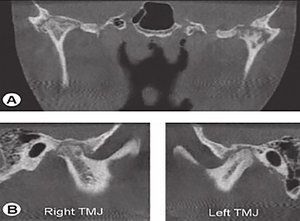
- Osseous changes are best viewed with CT. Cone beam CT also provides high-resolution, multiplanar reconstruction of the TMJ, with a low radiation dose.
- MRI is a noninvasive technique, considered to be the gold standard in imaging the soft-tissue components of the TMJ. MRI is useful in the evaluation of the articular disc and when looking for early signs of TMJD, such as the presence of joint effusion.
- High-resolution ultrasonography is a noninvasive, dynamic, inexpensive imaging technique, which can be useful in diagnosing TMJ disc displacements. The main issue with high-resolution ultrasonography is that this procedure is dependent on the examiner's skill and the quality of the equipment.
Imaging Considerations: Advantages and Disadvantages
The clinical examination is the most important in the diagnosis of TMJ pathology, but special imaging is necessary to make the appreciate diagnosis. In general, if there is joint locking, pain and articular sounds, imaging is recommended. When imaging the TMJ, it is important to also evaluate joint function. This is accomplished by comparing the condyle in the closed- and opened-mouth position.

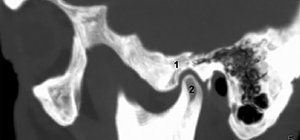
Panoramic Radiography: In the past, it was common for these patients to be evaluated utilizing panoramic radiography, typically in the dental office. The panoramic view demonstrates the jaws and the associated structures. This view is helpful in identifying any periodontal or odontogenic causes for orofacial pain. However, this view only demonstrates the lateral part of the condyle due to the superimposition of the zygomatic arch and the base of the skull. (Fig. 1)
Panoramic radiography does not assess the functional status of the TMJ. It only demonstrates late stages of degenerative bone changes, asymmetries of the condyles, fractures and osseous tumors. Panoramic radiography does not demonstrate the functional status of the joint, and has a relatively low specificity and sensitivity when compared with CT, which is more suitable for identifying TMJ changes than conventional radiography.
The main disadvantage of CT, compared to other radiological methods, is the cost, the radiation exposure and the visualization of the soft tissues. The disc, synovial membrane, ligaments, lateral pterygoid muscles are better evaluated with other imaging techniques.
Cone beam CT, introduced in the 1990s, is a modality that can be available in a dental practice. The main advantage of cone beam CT, compared to CT, is the lower radiation dose to the patient. The spatial resolution of cone beam CT is also higher than that of conventional CT.9 (Fig. 4)

Magnetic Resonance Imaging: MRI is currently considered the reference method for imaging the soft-tissue structures of the TMJ (articular disc, synovial membrane, lateral pterygoid muscle). MRI can detect the early signs of TMJ dysfunction, such as thickening of anterior or posterior band, rupture of retrodiscal tissue, changes in shape of the disc, and joint effusion. Images can be obtained in all planes (sagittal, axial, coronal). In most scanning sequences, T1-weighted, T2-weighted and proton-density (PD) images are obtained. (Fig. 5)
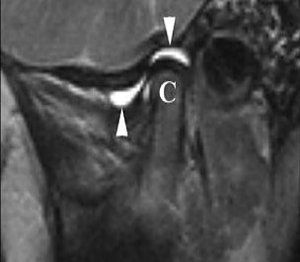
The PD images serve to visualize the disc-condyle relationship, while T2-weighted images are used in diagnosing inflammation in the joint. (Fig. 6) The slice thickness is important for image quality. The most frequently used section thickness is 3 mm. Reducing the slice thickness improves the quality of the images, but requires longer scanning time.10
Disadvantages of MRI examination include cost; time required; patients with claustrophobia have a difficult time; there is a possibility of missing the portion of condyle having a pseudocyst; and osseous pathology can be missed. This is when CT is the preferable imaging modality.

Regarding degenerative changes of the TMJ, ultrasound is still not recommended. One difficulty of US is the difficulty to obtain clear images, especially in the opened-mouth position, due to the overlying osseous structures. Another limitation of US is that the medial part of the disc cannot be visualized. The diagnostic value of high-resolution US is strictly dependent on the examiner's skills and the equipment used. There is a continuous need for trained and experienced professionals in this field.12
Clinical Takeaway
Selection of the proper radiological technique for evaluating the TMJ must be carefully made by the practitioner, in order to correlate the clinical signs and symptoms with the appropriate diagnosis. CT and MRI are currently the most used imaging techniques. CT is the most efficient examination in detecting osseous changes, whereas MRI remains the gold standard for articular disc examination.
High-resolution ultrasonography is also an important option in assessing the TMJ disc position, but is only useful when performed by an experienced practitioner with state-of-the-art equipment.
Chiropractors who treat TMJ disorders have been successful in managing this musculoskeletal condition conservatively. However most health care professionals and even patients do not consider chiropractic as a conservative option for TMJ problems. This bias needs to change. It is my intention to encourage chiropractors who are treating patients with TMJDs to document their results so it can enhance the data that's already been published.
References
- Prevalence of TMJD and Its Signs and Symptoms. National Institute of Dental and Cranialfacial Research.
- DeVocht JW, et al. A pilot study of a chiropractic intervention for management of chronic myofascial temporomandibular disorder. J Am Dent Assoc, 2013 Oct;144(10):1154-1163.
- Pavia S, et al. Chiropractic treatment of temporomandibular dysfunction: a retrospective case series. J Chiropr Med, 2015;14(4):279-284.
- Fuhr AW. The Activator Method, 2nd Edition. St Louis: Elsevier, 2009; pp. 336-355.
- Maluf SA, et al. Global postural reeducation and static stretching exercises in the treatment of myogenic temporomandibular disorders: a randomized study. J Manipulative Physiol Ther, 2010;33(7):500-507.
- Gemmell H, Allen A. Relative immediate effect of ischaemic compression and activator trigger point therapy on active upper trapezius trigger points: a randomised trial. Clin Chiropr, 2008;11:175-181.
- Blikstad A, Gemmell H. Immediate effect of activator trigger point therapy and myofascial band therapy on non-specific neck pain in patients with upper trapezius trigger points compared to sham ultrasound: a randomised controlled trial. Clin Chiropr, 2008;11:23-29.
- Palaskar JN, et al. Centric relation definition: a historical and contemporary prosthodontic perspective. J Indian Prosthodont Soc, 2013 Sep;13(3):149-54.
- Caruso S, et al. Temporomandibular joint anatomy assessed by CBCT images. Biomed Res Int, 2017;2017:2916953.
- Bag AK, et al. Imaging of the temporomandibular joint: an update. World J Radiol, 2014;6(8):567-582.
- Habashi H, et al. Dynamic high-resolution sonography compared to magnetic resonance imaging for diagnosis of temporomandibular joint disk displacement. J Ultrasound Med, 2015;34(1):75-82.
- Henderson RE, et al. Current and prospective use of musculoskeletal diagnostic ultrasound imaging at chiropractic teaching institutions: a worldwide survey of diagnostic imaging staff. J Chiropr Med, 2017;16(1):54-63.



