Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
Inflammatory Process of the Symphysis Pubis
Degenerative changes involving the symphysis pubis are a common radiographic finding. Many times we must decide if the changes seen are degenerative or inflammatory. The clinical history is extremely important when attempting to differentiate the changes seen in this region. Local bacterial infection can occur; however, the cause is usually due to systemic disease such as chronic hematogenous osteomyelitis, tuberculosis or even tertiary syphilis. Most of these disorders are not typically seen in practice. There is, however, an entity called osteitis pubis which appears radiographically similar to infection; however, no bacteria or virus has ever been isolated with this process. Osteitis pubis is not an uncommon complication in patients who have undergone a prostatectomy. The discomfort in the symphysis usually starts between four to 12 weeks after the prostatectomy. This disorder is also seen following vaginal deliveries, inguinal herniorrhaphy, abdominosacral extirpation of the rectum, abortion, blunt injury to the pelvis, and athletic injuries.
The pain may be accompanied by a rise in temperature and an elevated sedimentation rate; it also may radiate to the inguinal region and the medial aspect of the thigh. Chronic damage related to excessive strain at the origin of the gracilis, adductor longus, and adductor brevis muscles seen in athletes also will cause osteitis pubis, but this entity is often referred to as the gracilis syndrome, os pubis syndrome or posttraumatic osteonecrosis of the pubis.
Radiographically, the changes seen in osteitis pubis occur in several phases. Initially, the margins of the symphysis appear hazy due to diffuse demineralization of the subchondral bone from hyperemia. As this demineralization continues to occur, the symphysis appears to widen. Erosion of the margins of the bone begins to occur; usually this process is self-limiting. In the reparative phase increased density of the subchondral bone occurs with proliferative changes at the symphysis. Usually, once this process occurs, the synostosis has healed. The whole process usually occurs over a period of six to eight weeks, but symptoms can last as long as six months.
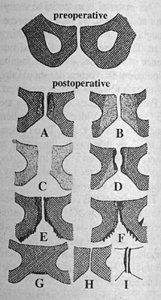
Osteitis pubis: clinical courses, end stages
A -- Symphysial contours ill-defined. In the subchondral space diffuse, in part spotty, demineralization and hazy structures of cancellous bone.
B -- The changes depicted in A, especially decalcification, have extended as far as the ischium.
C -- Considerable decalcification giving rise to "widening of the symphysial cleft."
D -- Erosion as direct cause of A and B.
E -- Repair stage recognizable by increase in density of the subchondral cancellous bone. In addition, bony trabeculae grow into the symphysial cleft, which has been narrowed by the increase in density. Roentgen manifestations of productive fibro-osteitis in the ischium.
F -- Progression of E.
G -- Healing by synostosis (may also develop directly after D).
H -- Except for narrowing of the symphysial cleft, the picture has returned to normal (for example, directly after C).
I -- Degenerative lesions of the symphysis as a late condition (e.g., after A through D).
Deborah Pate, D.C., DACBR
San Diego, California



