Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
Day in the Life of an Advanced-Practice DC
Can you tell us a little about your background in the profession? Why did you want to become a DC? I studied at Boston University from 1968-1972 as a pre-med student majoring in biology. Late in my junior year, I decided I was not going to pursue medical school. Five years after graduation, I discovered massage and Rolfing, and wanted to pursue both. I was more interested in a wholistic, rather than allopathic, approach to healing.
I became licensed in massage in Florida in 1977, but the Rolf Institute turned down my application. Unbeknownst to me, a chiropractor from Florida who was on the Rolfing Institute board knew about me and set out to enroll me in the chiropractic profession. When he explained it and I experienced it, I realized chiropractic was a match for a career. Within a few months I had set out from Florida to be one of 25 students in the inaugural class of Pacific States Chiropractic College in San Lorenzo, Calif.
Soon after school began in March 1978, the college broke apart over a highly contentious straight vs. mixer controversy and we (by then 40 students, plus administration and faculty) left and formed Northern California College of Chiropractic. In 1980, NC3, as we fondly called it, was bought out by Palmer College and became Palmer West. Pacific States was subsequently bought out by Life and became Life West.

What I liked initially about the profession was that it was a hands-on healing discipline accepted by patients and insurance companies, and that it appeared a good living could be made. I liked that the degree conferred was a doctorate. I liked the idea of helping people without resorting to drug treatment as a first choice. What I fully recognized and did not like, but accepted, was the fact that what constituted the "philosophy" was merely a dogmatic belief system not completely backed by sound science. I felt that in time, chiropractic would correct its unscientific nature, stop promising the world, and through rigorous testing, prove its efficacy.
I was first licensed in New Mexico in November 1981, then in California in January 1982. I practiced for a year in Northern California, then moved to Santa Fe, N.M., and opened my office in March 1983, where I have been practicing very successfully ever since.
What spurred you to advocate for and then pursue advanced-practice certification? Given the politics of my chiropractic education, I naturally gravitated to political involvement in New Mexico by becoming the northeast district director for the New Mexico Chiropractic Association in June 1983. I strongly felt part of my success was going to depend on my involvement in not only my practice, but with my colleagues in the state association. I have maintained that involvement in various positions for the past 33 years, including appointment to the state board of chiropractic examiners in 2010. In 2006, our association, which had a legislative committee of one, prudently created a PAC and I was appointed chairman.
Although early in my career, I had chosen not to become a homeopath, I still liked the results personally from various homeopathic remedies, and used some of them in my practice. When one of my homeopathic reps told me their product could be used as an injectable, I was excited about the possibilities. I figured that if the topical worked well, placing the product at a more precise location with an injection could work better.
Realizing that in order to do so required changes to our statute in New Mexico, we on the PAC set out to explore the possibility. The bigger issue, though, had to do with our status as physicians. Although insurance code held that we were, we discovered what really mattered was whether we were listed in the pharmacy acts, which we weren't. A listing in the pharmacy acts, along with all the other professions that had prescriptive privilege, was necessary to be able to use the injectable or any other prescription product.
We began to explore products that would have great effect with treatment of neuromusculoskeletal conditions, such as procaine or sarapin, and IV use of vitamins and minerals, which would open up possibilities within functional medicine.
It is important to note that not once did we ever think of replacing chiropractic with any of these procedures. We saw these could be adjunctive to chiropractic and contribute to a patient's success with their treatment program.
Although I had started my education and initial practice with the idea the chiropractic adjustment was all that was needed, I was able to [expand] that point of view to include other non-adjustment procedures, simply because our scope of practice allowed for efficacious treatment modalities that complement and assist the adjustment, as well as being able to provide our patients with a more comprehensive treatment regimen for their benefit. I fully believed, and still do, that the injection of a natural substance to augment an adjustment is essentially the same as the use of any other modality or the provision of a supplement to augment an adjustment.
I do realize an injection appears to be incongruous with an adjustment, but in my opinion, it isn't as long as a chiropractic physician is not stuck in chiropractic philosophical dogma. I liked, and still do, being able to give my patients additional treatment options that have proven to be enormously helpful.
In 2007, we introduced a bill that included changes to statute allowing licensed chiropractic physicians in New Mexico, with additional education, to prescribe, administer and dispense certain medications. This bill almost made it through to the governor's desk, but fell short at the last step. In 2008, we introduced it again and it went to the governor's desk and was signed, initiating the Advanced Practice Certification Act.
We then went through a process of formulary creation, which was at times a contentious engagement with the pharmacy and medical boards. We also introduced and got signed legislation in 2009 to redefine the formulary section of the statute, which wound up getting misinterpreted years later, hindering our progress. We have introduced a couple of advanced-practice bills, one in 2011 for plenary licensure that almost made it through and another in 2013, which we were not able to move forward.
In New Mexico, what are the educational requirements for certification and what are you entitled to do beyond the standard DC degree? The educational program to acquire Advanced Practice Certification in New Mexico sunset on Dec. 31, 2012. The law states that the educational program required beyond that date is a graduate degree in a chiropractic clinical practice specialty. What was required from 2008 through 2012 was, for those who had completed three years of postgraduate clinical chiropractic practice, a minimum of 90 clinical and didactic contact course hours in pharmacology, pharmacognosy, medication administration and toxicology certified by an examination from an institution of higher education approved by the New Mexico Board of Chiropractic Examiners and the New Mexico Medical Board. In addition, one had to have an advanced-practice chiropractic certification by a nationally recognized credentialing agency providing credentialing.
Our law goes on to state that a certified advanced-practice chiropractic physician may prescribe, administer and dispense herbal medicines, homeopathic medicines, vitamins, minerals, enzymes, glandular products, naturally derived substances, protomorphogens, live cell products, gerovital, amino acids, dietary supplements, foods for special dietary use, bioidentical hormones, sterile water, sterile saline, sarapin or its generic, caffeine, procaine, oxygen, epinephrine, and vapocoolants.
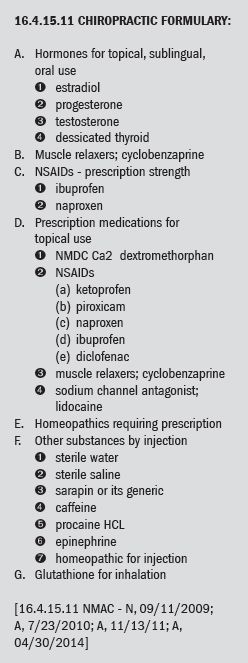
The law further states that a formulary shall be developed by the New Mexico Board of Chiropractic Examiners and approved by the New Mexico Medical Board and the Board of Pharmacy. I've included the entire formulary, as amended and intact from 2010 and currently active, below. To see the entire set of rules for chiropractic in New Mexico, click here.
In summary, all of the substances in the formulary, given the nature of administration, are prescription substances and require the advanced-practice certification for their use. All of the procedures available for use of the above substances are beyond the statutes of every other state, although there are a few states that have interpreted their statute and/or their rules in order to perform treatment similar to what is being done in New Mexico using some of the substances in the formulary.
At this time, additional items have been proposed to the New Mexico Board of Chiropractic Examiners for their approval. That process is not complete.
What's the average "day in the life" of an advanced-practice DC? I have been in practice for the past 34 years, the past 33 in Santa Fe. I see anywhere from 20-30 patients a day and work a three-day week. My primary interest is neuromusculoskeletal conditions.
I see typical chiropractic patients who present with everything from headache and neck pain, to lower back and hip pain. I deal with all joints of the body except for cranial. I do not practice functional medicine, so I do not attract patients with organic complaints and disease processes that may be amenable to that kind of treatment. I treat complex cervical and lumbar discopathies, neurogenic issues, extremity paraesthesias, etc.
My primary treatment is the chiropractic adjustment, which has been my treatment focus for my entire career. My primary protocol is evidenced based, unlike the subluxation-based practitioners who appear to care little for evidence beyond their detection of subluxation. I do fully believe that the chiropractic adjustment can be the best option for successful treatment, but I do not believe it has to be the only treatment. Once a licensed chiropractic physician starts to utilize what is in their repertoire, based on their education and scope of practice, their focus shifts from the adjustment to the patient's needs, with the adjustment being just one, albeit a very important one, of the many modalities that can be used to the patient's benefit.
I evaluate my patients using standard examination procedures learned in chiropractic school and in postgraduate seminars. I do not take X-rays as a matter of course – only if the presenting complaints and history are unusual or if treatment, after a week or so, is not working. I have an ultrasound machine which I use on occasion. I utilize a massage therapist as an adjunctive treatment, but not as an every-patient-gets-a-rubdown pre-chiropractic adjustment treatment. I do not spend time with cold or heat therapy prior to adjustment.
Every first visit for a new patient includes treatment. Report of findings occurs for me during the exam and treatment process, in which I am explaining and teaching as I proceed. I offer no custom brochure in which I mark off the affected vertebra, nor do I speak about vertebral subluxation. Instead, my education centers around joint dysfunction and the effects thereof.
I correct my patients on their use of the phrases "My bone went out," "Pop me back in, Doc" and "I adjusted myself" by explaining that none of that actually exists or happens; that those come from antiquated, historical chiropractic concepts. My explanation of joint dysfunction instead of vertebral subluxation is always greeted with, "Now I understand much better how chiropractic works."
I use medications such as topical prescriptions for pain management, Flexeril for muscle relaxation, and prescription-strength ibuprofen and naproxyn as anti-inflammatories, always judiciously. When a patient presents with severe pain that is going to require anywhere from a few to a handful of adjustments before their pain reaches tolerable levels, a prescription-strength NSAID can help augment and support the effects of the chiropractic adjustment. A similar patient, usually one from a new auto accident, may require a muscle relaxant taken over a few nights to provide necessary sleep for healing, especially if they have been having difficulty getting sleep. Topical prescription-strength medicines provide temporary relief to soft tissues between chiropractic adjustments.
In the eight years I have been able to write prescriptions, I am only in the middle of my second Rx pad of 50. I have been personally thanked by those patients who have benefited from the medications I have prescribed. I always explain what I am about to prescribe and why, in exactly the same way as I explain the plan of chiropractic treatment. I have never had a patient wonder why I, as a chiropractic physician, am giving them a prescription medicine. No one has ever told me that I "can't do that" because I am a chiropractor. All of the patients over the past eight years have followed my treatment plan and advice because I am a doctor who just happens to provide chiropractic services.
I utilize injection procedures such as prolotherapy with procaine, sarapin, saline, and various injectable homeopathics, on acute and chronic rotator-cuff issues, and chronic knee, foot, ankle, hand, elbow, wrist, cervical, lumbar, sacroiliac joint, and hip issues. I have been trained by the Hackett Hemwall Foundation and the American Academy of Orthopedic Medicine in prolotherapy injection protocol and technique, and I have been personally trained by Jan Kerschott, MD, in biopuncture.
My success rate using injection techniques is about 90 percent. I count as successful a minimal reduction in pain ratings of 80 percent using the Visual Analog Scale.
All of these injection procedures I have performed have been for issues that either did not respond to chiropractic treatment or are not amenable to chiropractic treatment, in my estimation. An example of the latter is the gentleman with artificial knees, whose history and subsequently very successful injection treatment you can look up on my website. An extraordinary story. I always practice chiropractic adjustments first.
Describe billing / reimbursement issues relative to advanced practice if different from standard chiropractic practice. Most insurance companies I deal with, the exception being Blue Cross, do not pay me for the injection procedures. Blue Cross does not pay very well for these procedures, but at least it is willing to acknowledge that my scope has expanded and to pay me for that scope.
To the best of my knowledge, any prescriptions I write for prescription medicines, oral or topical, are covered by a patient's insurance if their policy covers prescription medicines. If the patient has a $20 copay for their prescription from an MD, it is the same co-pay when prescribed by me.
Just as there are patients in a chiropractic office who pay full price in cash for their treatment, so do many of my patients pay full price for injection procedures. Keep in mind that these patients are paying for services they feel are important and necessary for their well-being. Each injection patient is provided with an injection informed-consent form which outlines the procedure about to be performed and what they can expect, as well as worse-case scenarios (which, by the way, have never occurred – site infection, adverse reactions).
As an aside, I would like to mention that in New Mexico, OUM malpractice has not raised its rates one penny for advanced-practice certified chiropractic physicians over and above the rates for traditional chiropractic physicians. NCMIC offered us reduced coverage and then forced us to make up the rest by participating in the New Mexico Risk Management Pool. This was its way of sharing the risk it says we are. There have not been, to the best of my knowledge, any malpractice issues regarding any of the APCs in New Mexico since the program's inception in 2008.
Editor's Note: In part 2 of this interview, Dr. Perlstein addresses concerns some DCs have regarding prescribing privileges, how advanced practice meshes with "standard" chiropractic practice, and what readers should know about the American Academy of Chiropractic Physicians, for which Dr. Perlstein serves as president.



