Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
The Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is a relatively common, chronic, and disabling condition. This syndrome is typically characterized by nocturnal hand discomfort, finger paresthesias in the median nerve distribution, and thenar muscle atrophy. This condition is most frequently caused by compression of the medial nerve in the carpal tunnel. This disorder occurs most often between the ages of 30 and 60 and is two to five times more common in women than men. The dominant hand is affected frequently; however, 32 to 50 percent of cases occur bilaterally.
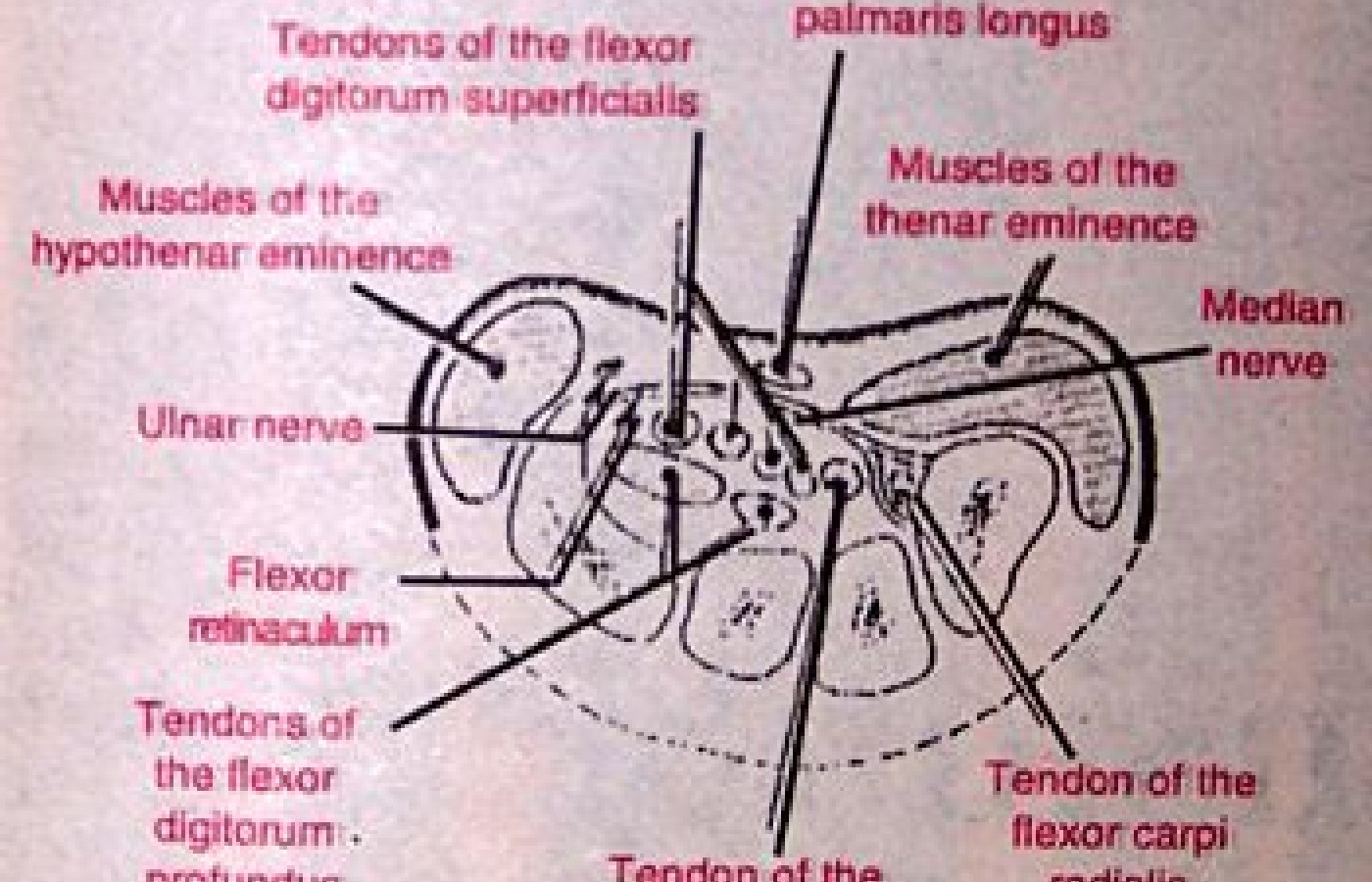
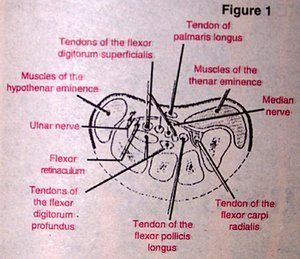
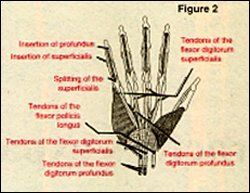
Anatomically, the carpal tunnel is formed by all the carpals of the wrist, which is deepened by the tubercles of the scaphoid and trapezium on the radial side and by the pisiform and hook of the hamate on the ulnar side. This concavity is converted into a tunnel by the tough flexor retinaculum which stretches between the tubercle of the scaphoid and ulnar styloid. The eight flexors of the fingers, the long flexor of the thumb, and the median nerve all share the space in the tunnel.
1. The local entrapment of the median nerve within the carpal tunnel can be classified into three groups:
a. The decrease in the size of the carpal tunnel due to bony or soft tissue changes such as misalignment of the carpal bones, fractures, dislocation, and hypertrophic osteophytes of fibrous scarring.
b. An increase in the volume of the normal content of the carpal tunnel. This can be due to occupational hypertrophy of the muscles and tendons in the carpal tunnel which is not uncommon in dentists, tennis, golf players, typists, factory workers, and persons confined to wheelchairs. Synovial proliferation due to arthritis, tenosynovitis, edema due to congestive heart failure, and amyloid in patients in dialysis are other less common causes for an increases in the content of the carpal tunnel.
c. Space-occupying lesions such as lipoma and ganglion cysts that also cause entrapment of the median nerve within the carpal tunnel.
2. Systemic diseases also will cause neuritis affecting the median nerve, most commonly patients with diabetes; seven percent of patients with CTS have diabetes.
3. The third cause of CTS has been labeled as iodiopathic, in fact 50 percent of patients with CTS have an unknown etiology. CTS has also been found in association with menopause and late trimester pregnancy.
The diagnosis of CTS until recently has been mainly empirical. Present diagnostic parameters include clinical history, clinical signs, and nerve conduction studies which can be equivocal. Imaging modalities prior to magnetic resonance imaging (MRI) have been in most circumstances non-contributory, with the exception of osseous lesions, such as fractures and osteophytes. Likewise, the choice of conservative or surgical treatment is largely empirical.
The reason for the success or failure of conservative treatment is poorly understood, possibly because the exact cause for the symptoms is generally not established prior to treatment. The role of MRI in the evaluation of carpal tunnel syndrome is presently not definitive because the parameters for conservative and surgical treatment have not been established.
Unfortunately for our patients, there is no generally accepted guide for when a patient should undergo surgery. Many times the patient undergoes surgery whenever the orthopedist feels the patient hasn't responded to conservative care. If there is no demonstrable cause of pressure on the median nerve, then conservative management should be the preferred treatment. Reasons for the failure of surgical treatment or recurrences of symptoms could be due to delayed treatment, inadequate incision of the flexor retinaculum, postoperative scar or neuroma, or a growing space-occupying lesion within the carpal tunnel. The diagnosis and treatment of CTS could be made substantially more objective with the use of MRI.
The location, swelling, and constriction of the median nerve can be easily assessed with MRI. Edema and fluid in tendon sheaths can also be seen with MRI. Ischemic necrosis of bone, incisional neuroma, and fat within the carpal tunnel can also be demonstrated. MRI can be used to assess the etiology of the patient's symptoms permitting a more rational choice of treatment options directed toward the etiology. Posttreatment MRI examination could also serve as a useful means in predicting the success or failure of a given treatment.
Deborah Pate, D.C., DACBR
San Diego, California