Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
Evaluate Orthopedic Hardware before Adjusting the Patient
DCs must exercise caution when adjusting patients with orthopedic hardware in the region intended for adjustment. The first consideration should be to assess if the region is stable. Orthopedic hardware can loosen - even fracture - due to biomechanical stresses and infection. We are very good at assessing biomechanical changes as they appear on plain films. However, we are not so familiar with the radiographic changes associated with orthopedic hardware; we should be aware of the problems associated with it, especially if we are going to treat patients with orthopedic fixation devices.
The most efficient way of assessing the stability of a fixation device is to take a radiograph. There are just a few simple key points to keep in mind when performing radiographs of orthopedic fixation hardware.
Technical Considerations for X-rays of Orthopedic Hardware
These should:
- expose a minimum of two orthogonal views of the body part;
- include the entire body part on the film, including the joints above and below;
- include the entire orthopedic device, preferably with several centimeters of normal bone on either end;
- include a slight overexposure, which may be helpful for looking at metal fixation devices; and
- be compared with old films, which is mandatory if there is a healing fracture.
Though these patients may already be managed by orthopedists, for general safety, the chiropractor should carefully look for problems of fixation. Specifically, look at the alignment, apposition and rotation of the region involved. Always look for problems with the fixation device, such as incorrect application of the device, device failure, or infection of the device.
Be familiar with the general names and function of the various orthopedic devices that our patients might carry with them. I am not suggesting that we need to know the specific manufacturer or model number of each device; just the general name and function the devices most commonly used, particularly in the spine and pelvis. If one is generally aware of the particular function of the device, evaluating the stability of the region is much easier. Avoid counter-rotation and the use of the area with the device as a fulcrum. This is just a general rule of thumb, but it makes sense not to stress an area that might be weak anatomically. One might need to modify or completely avoid some adjustment techniques.
Classification of Orthopedic Fixation Devices
Internal Fixation Devices
- screws
- plates
- wires and pins
- intramedullary rods and nails
- spinal fixation devices
- fracture fixation
- radius
- tibia
- pelvis
- bone lengthening
- Ilizarov device
First, as chiropractors we don't have to worry about the external fixation devices, because a chiropractor would not adjust a patient with these types of contraptions in place.
These are just a few examples of external fixation devices; fortunately, we don't need to discuss these. So, let's revise our list to the following:
- screws
- plates
- wires and pins
- intramedullary rods and nails
Screws: The mainstay of orthopedic fixation is the screw. There are many uses for the screw. It can be used alone or along with other devices. The general principle is that bone heals better if the fracture fragments are aligned and pressed closely together. The idea is to stabilize the fracture and keep the bone in anatomic alignment. Screws do not protect fractures from bending, rotation or axial loading forces. Other devices are used to provide these functions. The main function of the screw is to compress the fragments together. This can be static or dynamic (where the body's weight or muscle forces produce added compression).
Another type of screw commonly used is a cannulated screw, with a hollow shaft. The main advantage of this type of screw is that it can be placed very precisely. First, a wire is placed in the area of interest; then the cannulated screw is driven into the bone along the shaft of the wire. Then the wire is withdrawn. The problem with this technique is that it is possible to perforate the articular surface.
One should remember that in order to use a screw, one has to make a screwhole in the bone or in the hardware. It is estimated that one screwhole passing through both cortices of a femoral shaft will weaken that femur by 90 percent to some types of stress. We don't want to find out what types of stress those are, so stay away from those screws.
Washers are used in two situations: to distribute stresses under a screw; and serrated washers are used to affix avulsed ligaments, small avulsion fractures or comminuted fractures to the main bone.
Before we describe other devices, the most interesting screw of which I am aware is the one that is invisible to x-ray.

Wires
Generally referred to as the Kirschner or "K" wires, these are very handy devices. Besides their usage with cannulated screws, they are used in many other ways to help reduce and stabilize fractures. A K wire is essentially an unthreaded segment that is drilled into bone like a drill bit. The major advantage of a K wire is that it is very small and relatively noninvasive, as hardware goes. It can be placed through an articular surface, or even across an open epiphyseal plate without injury. K wires can be used for either temporary or final stabilization. They can be placed between bones (as shown in Figure 8), or they can be used as an intramedullary device to bridge a fracture of a small tubular bone. They are commonly used to help piece together all of the fragments of a comminuted fracture prior to placement of the final fixation device, especially with an intraarticular fracture.

Plates
There are lots of plates used in orthopedics, and they are named according to their functions, such as compression, neutralization, and buttress plates.

Static compression refers to the production of axial compression along cortical fractures with the potential advantages of more rigid fixation. The problem with this procedure is that it requires a longer surgical incision, and there is a possibility of refracture after the plates is removed, due to the atrophy that occurs beneath the plate.
A dynamic compression plate has screwholes with sloped sides that correspond to the lope of the under surface of the screw. As the screws are tightened, the screw head glides down the incline of the screw hole, toward the center of the plate. This procedure is used for treatment of comminuted and segmented fractures.
Neutralization bridges a comminuted fracture and transmits bending or torsional forces from the proximal to the distal fragment, protecting the intervening fracture fragments from these forces.
The sliding screw plate apparatus consists of a lag screw and a slide plate with a barrel. The threaded portion of the screw is placed in the femoral head and its shaft is inserted into the barrel of the side plate. The threads of the lag screw should be in the subchondral bone, with the screw tip optimally about one half inch from the articular surface. The side plate should lie flush with the femoral shaft and the screws attaching it to the cortex should just penetrate the far cortex. The barrel of the side plate should not contact the proximal fracture fragment to ensure impaction of bone at the fracture site.
The degree of telescoping of the sliding screw is measured by noting the change in the distance from the end of the barrel to the first screw thread on the initial radiographs, in comparison to the most current examination. Telescoping usually averages 7mm. 7mm on leg length discrepancy can cause significant biomechanical changes in the pelvis and low back. Keep this in mind when treating any patient with a previous hip fracture.
As with any device, several complications can occur; the screw can penetrate the joint; the lag screw turns out to be too short and the telescoping may be limited by contact between the threaded portion of the screw and the barrel. The telescoping mechanism may also fail due to other reasons: The nail may break or bend caused by nonunion of the fracture; the screw can become disengaged from the barrel. In other words, this is not a foolproof mechanism, as with any device. complications can occur. Before manipulating any patient with any orthopedic hardware, make certain there is nothing wrong with the placement and stability of the device. Then be certain the technique used is not going to affect the stability of the region.

Rods
There are a large variety or devices that can be placed into the intramedullary canal. Two of the most common are the interamedullary rod and the interamedullary nail. Any of these devices can be generally divided into two groups; by whether intramedullary reaming is necessary prior to placement of the device. The nails to be placed in the medullary canal must first have the canal reamed so as not to shatter the bone as the nail is hammered down the shaft. Reaming also has its problems such as thermal osteonecrosis, compromising the blood supply. If intraosseous pressure becomes elevated during the process, fat emboli can migrate to lungs. Therefore, as you might suspect, if reaming can be avoided, it is the preferred technique, so there are several devices developed for insertion without reaming the canal. The "rush" rod has a chisel-like tip, and is commonly used for fibular shaft fractures. Another type of unreamed nail is the Ender nail, which also has a chisel-like end and can be used three or four at a time.

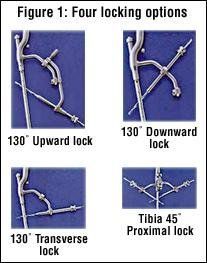
Lastly, let us just review some of the common spinal fixation devices. The prototype for spinal fixation is the venerable Harrington rod. It is used for either distraction or compression, and has hooks on either end that are designed to be placed under the lamina or traverse processes; then the device is either extended or compressed. Often they are used in conjunction with each other, and one side is compressed while the other side is extended, as in the scoliotic spine. I'm certain you have all seen these types of devices.
Other common devices are Weiss springs, which are compression devices that are attached to the laminae. Luque rods are L-shaped, or rectangular rods that are attached to the spine by a series of wires placed around the laminae. These provide considerable stability so that the need for postoperative immobilization is reduced.

Again as with any device, it can fail, and the above are a few examples of fractured Harrington rods.
I have given you a glimpse of the various types and functions of orthopedic hardware. It is not important to remember the specific names, but only the basic functions of the types of devices. If we use caution when managing patients with hardware, we will avoid causing any more injury and may even affect some relief in clinical symptoms.
Deborah Pate,DC,DACBR
San Diego, California
patedacbr@cox.net



